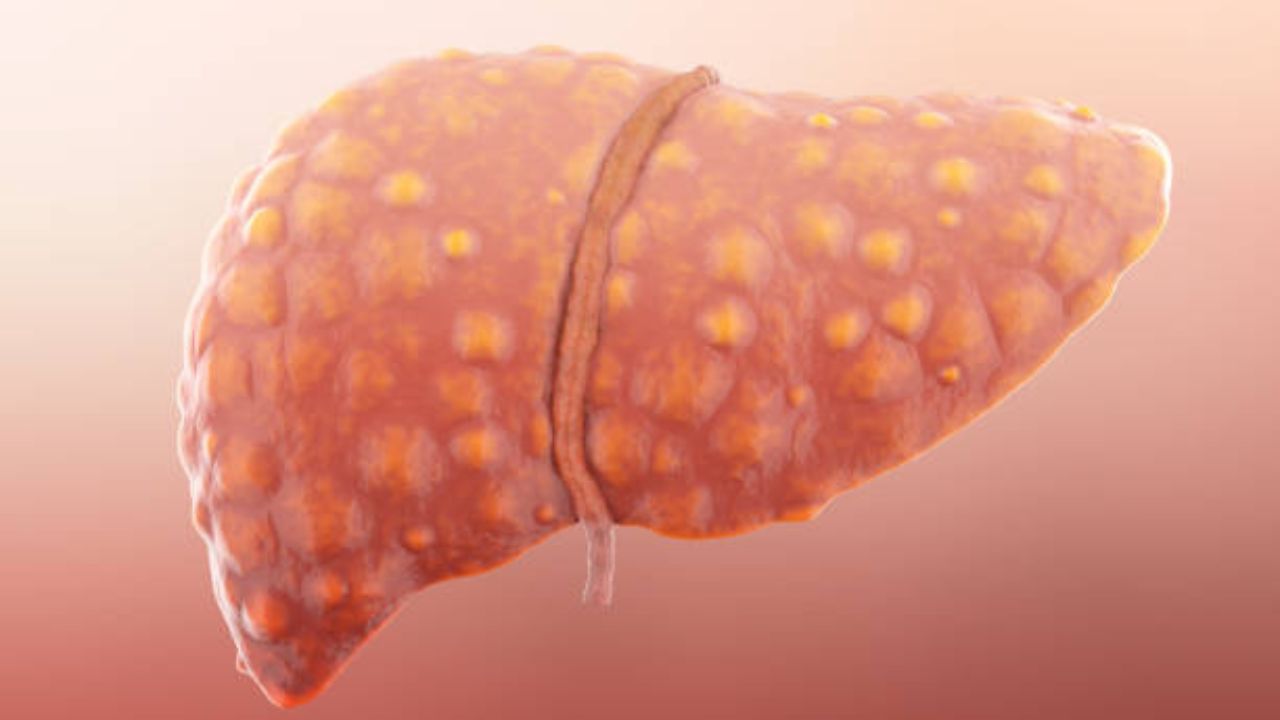
Alcoholic hepatitis is a very severe inflammatory attack of the liver, caused by excessive alcohol consumption. Often asymptomatic, it can have serious consequences.
What is alcoholic hepatitis?
Hepatitis is an inflammatory disease of the liver which consists of severe damage to the liver. It is characterized by the development of lesions associated with the death of liver cells which alter its functioning and its biological parameters. There are several forms. Hepatitis can be caused by a virus, this is the case of hepatitis A, B and C for example. It can also have other causes such as the accumulation of fat in the cells of the liver unrelated to alcohol (we speak of non-alcoholic fatty hepatitis) or the consumption of alcohol. It is the latter that is in question here.
There are two types of alcoholic hepatitis:
- Acute, brutal hepatitis, immediately after massive alcohol intoxication. Most often symptomatic, it can be extremely serious. This type of hepatitis is very rare in Europe.
- Chronic hepatitis that develops over time with excessive and regular alcohol consumption. It can be punctuated by more acute episodes. Hepatitis can then progress to cirrhosis and be associated with a risk of short-term mortality. This is the most common type in USA.
Since alcoholic hepatitis is most often asymptomatic, it is difficult to assess its prevalence. It would affect 1 excessive drinker out of 5. It is associated with liver failure and a high mortality rate.
What are the causes of alcoholic hepatitis?
The most common cause of hepatitis is alcohol abuse. Drinking alcohol in moderation is advised for a good reason. Indeed, alcohol is a poison for the organism. In small doses, it is filtered by the liver and evacuated. In high doses, alcohol damages several organs: the digestive tract which absorbs it, the kidney which filters a small part of it and evacuates it in the urine, the lung which evacuates a small part of it in the exhaled air and finally the liver which filters the vast majority (90%) of the alcohol absorbed. The liver gets tired and can eventually get sick and no longer be able to perform its functions properly. Alcohol toxicity on the liver can occur at doses that may appear low: 20 to 40 grams of alcohol per day, i.e. 2 to 4 glasses in women and 40 to 60 grams of alcohol per day,
The consequences for the liver are as follows, in order of severity:
- Steatosis or alcoholic hepatitis: fat is deposited in liver cells.
- Hepatomegaly: the volume of the diseased liver increases.
- Fibrosis: inflammation of the liver leads to the formation of scar tissue.
- Cirrhosis: the liver tissue continues to change and becomes hard.
- Liver cancer.
These four types of lesions can be observed simultaneously or in isolation. Steatosis and hepatomegaly may be reversible if alcohol consumption is stopped immediately.
The risk of developing alcoholic hepatitis is higher in women than in men. This risk is increased in case of overweight or obesity. There is also a genetic predisposition.
What are the symptoms of alcoholic hepatitis?
Alcoholic hepatitis can be asymptomatic for a very long time and manifest itself only at an already advanced stage. When symptoms appear, it may be:
- Jaundice: yellow coloring of the skin, eyes and certain mucous membranes due to an accumulation of bilirubin (product of breakdown of red blood cells normally filtered by the liver and evacuated by the urine, for which it is responsible for the coloring).
- Ascites: increase in the volume of the abdomen due to hypertension in the veins bringing blood to the liver.
- Hepatic encephalopathy: neurological disorders due to brain damage secondary to liver dysfunction.
Risk factors
- Drinking large amounts of alcohol.
- Drinking alcohol for a long time.
- Female.
- Having a genetic predisposition to alcoholic liver disease.
- Obesity or underweight.
Alcohol abuse can cause three types of liver damage, which often develop in the following order:
- Fatty degeneration of the liver or liver steatosis.
- Alcoholic hepatitis.
- Cirrhosis of the liver.
Possible Complications
- Wernicke’s encephalopathy.
- Korsakov’s syndrome (memory loss, disorientation)
- Coma.
- Anemia.
- Ascites (accumulation of fluid in the abdomen).
- Portal hypertension.
- Internal bleeding
- Development of hepatorenal syndrome, manifestation of severe renal failure.
- Development of the hepatopulmonary syndrome.
- Menstrual dysfunction in women.
- Development of hepatic gastropathy and colopathy (disease of the gastrointestinal tract).
- Liver cancer.
Diagnosis
Taking into account the manifestations of the disease, the severity of the course and concomitant factors, the doctor may prescribe the following types of examination:
- General and biochemical blood tests.
- Urine tests.
- Analysis of feces for occult blood.
- Liver biopsy.
- Ultrasound examination of the abdominal organs.
- Computed tomography (CT) of the liver.
- Magnetic resonance imaging (MRI) of the liver.
How to treat alcoholic hepatitis?
The first stage of treatment is the reduction, or even the total cessation of alcohol consumption. In the event of addiction, follow-up in an addiction service and/or by a psychologist can be set up. There are drug treatments to accompany withdrawal.
Weaning can be accompanied by diuretic treatment if necessary. The patient may also receive a vitamin supplement. Treatment with corticosteroids can be put in place to reduce inflammation.
After weaning and treatment, in case of non-repairable damage inflicted on the liver, it is possible to consider a transplant. Patients eligible for transplantation are rigorously selected and the absence of alcohol consumption is a prerequisite.
The mortality rate for alcoholic hepatitis remains high. Indeed, the therapeutic alternatives are not numerous. The disease is often accompanied by serious infections and malnutrition. The risk of relapse in the event of addiction also remains high.
