Many people want to know if Alzheimer’s can be hereditary, especially if there is a family member affected. But only in very few cases is Alzheimer disease hereditary. The age-related form of the disease is much more common.
ICD codes for Alzheimer’s disease: F00G30
Alzheimer’s: brief overview
- What is Alzheimer’s? The most common form of dementia, affecting around 20 percent of people over the age of 80. Differentiation between pre-senile (< 65 years) and senile Alzheimer’s (> 65 years).
- Is Alzheimer disease hereditary?: Only about one percent of all Alzheimer’s cases are clearly hereditary.
- Causes: Death of nerve cells in the brain due to protein deposits.
- Risk factors: Age, high blood pressure, elevated cholesterol levels, vascular calcification, diabetes mellitus, depression, smoking, few social contacts, genetic factors.
- Early symptoms: dwindling short-term memory, disorientation, difficulty finding words, altered personality, weakened immune system.
- Diagnostics: by combining several tests, a doctor’s consultation, brain scans using PET-CT or MRT, CSF diagnostics.
- Treatment: no cure, symptomatic therapy with antidementia, neuroleptics, antidepressants; non-drug therapy (eg, cognitive training, behavioral therapy).
- Prevention: healthy nutrition, regular exercise, memory, many social contacts.
What is the Alzheimer’s disease?
Alzheimer’s is the most common form of dementia. The slowly progressing brain disease leads to memory loss, confusion and disorientation. Alzheimer’s cannot be cured, but it can be alleviated and slowed down.
Hereditary Alzheimer’s disease
Only about one percent of all Alzheimer’s cases are clearly hereditary. Three genes are known to be responsible for this form. If one of these genes has mutations, Alzheimer’s disease will break out in any case. Those affected usually fall ill very early, between the ages of 30 and 65. The disease is inherited in an autosomal dominant manner, which means that if one parent is affected, there is a 50 percent chance that the children will also be affected. This inherited form is also called “familial” Alzheimer’s disease.
In 99 percent of all Alzheimer’s diseases, age is the greatest risk of developing the disease. The symptoms usually only begin after the age of 65. However, there seems to be a genetic influence here as well. The change in the gene apolipoprotein epsilon 4 (ApoE4) increases the risk of the disease, even if it does not lead to a definite outbreak. The ApoE4 gene could play a role in up to 25 percent of all Alzheimer’s cases. Additional genes have been identified that may increase the risk of Alzheimer’s. Age-related Alzheimer’s disease is also called “sporadic”.
“The changes in the brain do not differ in the sporadic and familial form of Alzheimer’s. In addition, the course of both variants is very similar. This suggests that the disease mechanisms of the rare familial forms and the common sporadic Alzheimer’s disease are very similar.”
The most important differences at a glance:
The hereditary Alzheimer’s disease
- Rarely (about one percent of all cases)
- Early age of onset between 30 and 65 years
- Causative mutation in three genes: APP (chromosome 21), presenilin-1 (chromosome 14) and presenilin-2 (chromosome 1)
- Autosomal dominant inheritance
- Those affected will get sick in any case
Age-related Alzheimer’s disease
- Very common (about 99 percent of all cases)
- Late age of onset from 65 years
- Age is the most important risk factor
- Less influence of genetic factors
- Gene involved: Apolipoprotein Epsilon 4 (ApoE4) and other gene variants
Alzheimer’s: causes and risk factors
In the brains of Alzheimer’s patients, nerve cells and the connections between them gradually die off. As a result, the brain shrinks by up to 20 percent: the convolutions on the surface of the brain deepen and the cerebral ventricles expand. The destruction of the nerve cells begins in the so-called olfactory bulb. It then spreads to brain regions responsible for memory. Eventually it will cover the entire surface of the brain.
The Meynert basal nucleus is particularly affected by cell death at an early stage: the nerve cells in this lower-lying brain structure produce the neurotransmitter acetylcholine. Cell death in the Meynert basal nucleus thus triggers a significant acetylcholine deficiency. As a result, information processing is disrupted: those affected can hardly remember recent events. So your short-term memory is fading.
Protein deposits kill nerve cells
In the affected brain regions there are two different types of protein deposits that kill the nerve cells. Why these form is unclear.
Amyloid beta : Hard, insoluble plaques of amyloid beta form between nerve cells and in some blood vessels. These are fragments of a larger protein whose function is still unknown.
Normally beta amyloid is degraded. In Alzheimer’s patients, this clean-up process no longer works in the brain, so the protein fragment is deposited. This inhibits the energy and oxygen supply to the brain – nerve cells die.
Tau protein : In addition, abnormal tau fibrils – indissoluble, twisted fibers made of the so-called tau protein – form in the nerve cells of the brain in Alzheimer’s patients. They disrupt the stabilization and transport processes in the brain cells, causing them to die.
Alzheimer’s risk factors
The main risk factor for Alzheimer’s is age: only two percent of those under the age of 65 develop this form of dementia. In the 80 to 90 age group, on the other hand, at least one in five is affected, and among the over 90 year olds even more than a third suffer from Alzheimer’s.
But old age alone does not cause Alzheimer’s. Rather, experts assume that other risk factors must also occur before the disease breaks out.
Overall, the following factors can promote Alzheimer’s disease:
- Age
- Genetic causes
- High blood pressure
- Increased cholesterol level
- Increased level of homocysteine in the blood
- Arteriosclerosis (atherosclerosis)
- Poorly controlled blood sugar in diabetes
- Oxidative stress caused by aggressive oxygen compounds that play a role in the formation of protein deposits in the brain.
There are other factors that may increase the risk of Alzheimer’s, but more research needs to be done. This includes inflammation in the body that lasts for a long time: Researchers believe that it could damage brain cells and promote the formation of protein deposits.
Other possible risk factors for Alzheimer’s include a low level of general education, head injuries, brain infection by viruses and an increase in autoimmune antibodies in older people.
Aluminum & Alzheimer’s
Autopsies have shown that the brains of deceased Alzheimer’s patients have an increased concentration of aluminium. But that doesn’t necessarily mean that aluminum causes Alzheimer’s. Animal experiments speak against it: If you give mice aluminum, they still do not develop Alzheimer’s disease.
It is possible that increased aluminum levels are a consequence of the disease and not a cause of Alzheimer’s. Whether this is actually the case needs to be investigated in further studies.
Is Alzheimer disease hereditary?
just about one percent of all Alzheimer’s patients have the familial form of the disease: Alzheimer’s is triggered by various genetic defects that are passed on. Affected by the mutation are the amyloid precursor protein gene and the genes presenilin-1 and presenilin-2. Anyone who carries these mutations will definitely develop Alzheimer’s, and that between the ages of 30 and 60.
However, the vast majority of Alzheimer’s patients show the sporadic form of the disease, which generally only breaks out after the age of 65. It is true that the sporadic form of Alzheimer’s also seems to have a genetic component: This involves changes in the gene for the protein apo-lipoprotein E, which is responsible for transporting cholesterol in the blood. However, changes in this gene do not lead to the definite outbreak of the disease, but only increase the risk of it.
In general, the older someone is when Alzheimer’s develops, the less likely it is that it is a familial form. Relatives then usually do not have to worry that they may have inherited the disease.
Alzheimer’s: Symptoms
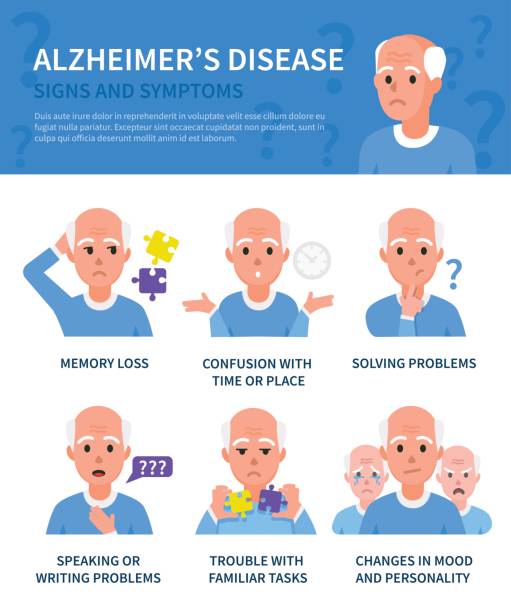
In the course of Alzheimer’s disease, the symptoms intensify and new complaints appear. Therefore, below you will find the symptoms arranged according to the three stages into which the course of the disease is divided: early stage, middle stage and late stage:
Alzheimer’s symptoms in the early stages
The first symptoms of Alzheimer’s are minor lapses in memory that affect short-term memory: for example, patients cannot find objects they have recently put away or cannot remember the content of a conversation. You can also “lose the thread” in the middle of a conversation. This increasing forgetfulness and absent-mindedness can confuse and frighten those affected. Some react to this with aggressiveness, resistance, depression or withdrawal.
Alzheimer’s can also sometimes be recognized by word-finding disorders, although there can also be other causes for such disorders. With a word-finding disorder, those affected sometimes no longer remember familiar terms.
Other early signs of Alzheimer’s can include slight orientation problems, lack of drive and slowed thinking and speaking.
With mild Alzheimer’s dementia, everyday life can usually be managed without any problems. Those affected often only need help with more complicated things, for example managing their bank account or using public transport.
Mid-stage Alzheimer’s symptoms
Alzheimer’s symptoms in the middle stages of the disease are aggravated memory disorders : the patients are less and less able to remember recent events, and long-term memories (e.g. of their own wedding) gradually fade. Familiar faces are becoming increasingly difficult to recognize.
Difficulties in orienting oneself in time and space also increase. For example, the patients are looking for their long-dead parents or can’t find their way home from their usual supermarket.
In addition, patients now need more and more help with simple activities such as cooking, combing their hair or bathing. An independent life is then hardly possible.
Communication with patients is also becoming increasingly difficult: those affected are often no longer able to form complete sentences. They need clear requests that often have to be repeated before they sit down at the dining table, for example.
Other possible Alzheimer’s symptoms in the middle stages of the disease are an increasing urge to move and severe restlessness. For example, patients may be walking back and forth restlessly or asking the same question over and over again. Delusional fears or beliefs (like being robbed) can also occur.
Late stage Alzheimer’s symptoms
In the late stages of the disease, the patients are completely in need of care. Many need a wheelchair or are bedridden. They no longer recognize family members and other people close to them. Speech ability is now limited to a few words. Eventually, patients can no longer control their bladder and bowels (urinary and fecal incontinence).
Increasing problems with chewing, swallowing and breathing as well as stiffening of the limbs are typical late-stage Alzheimer’s symptoms. Due to the weakened immune system, infections (e.g. pneumonia) often occur, which then often lead to death.
Atypical course of Alzheimer’s
In about a third of patients who develop the disease at a younger age (a small group overall), the course of Alzheimer’s is atypical:
- Some patients develop behavioral changes toward antisocial and conspicuous behavior that are similar to those seen in frontotemporal dementia.
- In a second group of patients, word-finding difficulties and slowed speech are the main symptoms.
- A third form of the disease involves vision problems.
Alzheimer’s: investigations and diagnosis
If you notice increasing forgetfulness in yourself (or in a loved one), you should consult a family doctor. If necessary, they will refer you to a neurologist, psychiatrist or memory clinic. Such an outpatient clinic is a department of a hospital that specializes in brain disorders. Various examinations are carried out there to get to the bottom of the suspicion of Alzheimer’s. So far, there is no single examination and no specific laboratory test that could be used to clearly diagnose Alzheimer’s.
Medical history collection
If Alzheimer’s is suspected, the doctor will first talk to you in detail to collect your medical history. He will ask you about your symptoms and any previous illnesses. The doctor will also ask about any medications you are taking. Because some preparations can impair brain performance. During the conversation, the doctor also pays attention to how well you can concentrate.
Ideally, someone close to you should accompany you to this doctor’s consultation. Because in the course of Alzheimer’s disease, the nature of those affected can also change. Phases of aggressiveness, suspicion, depression, anxiety and hallucinations can occur. Such changes are sometimes noticed more quickly than those affected themselves.
Physical examination
After the interview, the doctor will examine you routinely. For example, he measures the blood pressure and checks the muscle reflexes and the pupillary reflex.
Dementia testing
With a dementia test, simple exercises can be used to determine whether dementia is present. For example, you have to remember and repeat as many terms as possible from a word list with ten terms. Important dementia tests are the clock test, MMST (mini mental status test) and the DemTect (dementia detection test). However, it is not easy to identify dementia at an early stage. In addition, such tests do not allow differentiation between different forms of dementia (Alzheimer’s, vascular dementia, etc.).
In addition to the short tests mentioned, more detailed neuropsychological examinations are often carried out.
Apparative investigations
If there are clear signs of dementia, the patient’s brain is usually examined using positron emission computed tomography (PET/CT) or magnetic resonance imaging (MRI, also known as magnetic resonance imaging). In this way it is possible to find out whether the brain substance has decreased. This would strengthen the suspicion of dementia.
Imaging studies of the skull are also used to detect any other diseases that may be responsible for the symptoms of dementia, such as a brain tumor.
Laboratory tests
Blood and urine samples from the patient can also be used to find out whether a disease other than Alzheimer’s is causing the dementia. This can be, for example, a thyroid disease or a deficiency in certain vitamins.
Liquor diagnostics provide relatively reliable results : a sample of the cerebrospinal fluid (liquor) is taken from the lumbar spine (lumbar puncture) and examined in the laboratory. If the concentrations of certain proteins (amyloid protein and tau protein) in the cerebrospinal fluid are characteristically altered, there is a high probability of Alzheimer’s disease.
If the doctor suspects that the patient is suffering from the rare hereditary form of Alzheimer’s disease, a genetic test can provide certainty.
Alzheimer’s: treatment
There is only one symptomatic treatment for Alzheimer’s – a cure is not yet possible. However, the right therapy can help patients to be able to manage their everyday lives independently for as long as possible. In addition, Alzheimer’s drugs and non-drug therapy measures alleviate the symptoms of the patients and thus improve the quality of life.
Antidementia drugs
Various groups of active ingredients are used in drug therapy for Alzheimer’s:
So-called cholinesterase inhibitors (such as donepezil or rivastigmine) block an enzyme in the brain that breaks down the neurotransmitter acetylcholine. This messenger substance is important for communication between nerve cells, concentration and orientation.
In Alzheimer’s patients, insufficient acetylcholine is produced. In the early to middle stages of the disease, this deficiency can be compensated for for a while with cholinesterase inhibitors: this makes everyday activities easier for those affected. In addition, cognitive abilities such as thinking, learning, remembering and perceiving are preserved for longer.
In the case of moderate to severe Alzheimer’s dementia, the active ingredient memantine is often given. Like cholinesterase inhibitors, it can delay the decline in mental performance in some patients. To be more precise, memantine prevents an excess of the neurotransmitter glutamate from damaging the brain cells. Experts suspect that excess glutamate contributes to the death of nerve cells in Alzheimer’s patients.
Extracts of ginkgo leaves (Ginkgo biloba) are said to improve blood circulation in the brain and protect nerve cells. Patients with mild to moderate Alzheimer’s dementia may be able to cope with everyday activities better. In high doses, ginkgo also seems to improve memory and alleviate mental health problems, some studies show.
Other medications for Alzheimer’s
Alzheimer’s disease is often accompanied by psychological symptoms and behavioral changes, such as aggressiveness, passivity, restlessness or anxiety. If non-drug measures do not help, the doctor can prescribe so-called neuroleptics (such as risperidone or haloperidol).
However, these drugs can have serious side effects. These include an increased risk of stroke and increased mortality. The use of neuroleptics is therefore closely monitored. In addition, these drugs should be dosed as low as possible and not taken long-term.
Many Alzheimer’s patients also suffer from depression. On the other hand, antidepressants such as citalopram, paroxetine or sertraline help.
In addition, other existing underlying and concomitant diseases such as elevated blood lipid levels, diabetes or high blood pressure must also be treated with medication.
Non-drug treatment
Non-drug therapy measures are very important in Alzheimer’s disease. They can help to delay the loss of mental abilities and to maintain independence in everyday life for as long as possible.
For example, reality orientation training helps patients to find their way around in terms of space and time. Spatial orientation is supported, for example, by colored markings of different living spaces such as bathrooms and kitchens. Time orientation can be improved with the help of clocks, calendars and pictures of the current season.
Cognitive training can be particularly useful in the case of mild to moderate Alzheimer’s dementia: it can train the ability to learn and think. Simple word games, guessing terms or adding rhymes or well-known proverbs are suitable for this.
As part of behavioral therapy, a psychologist or psychotherapist helps patients to better deal with psychological symptoms such as anger, aggression, anxiety and depression.
Autobiographical work is a good way to keep memories of earlier stages of life alive : relatives or carers ask Alzheimer’s patients specifically about their earlier lives. Photos, books or personal items can help to evoke memories.
Occupational therapy can be used to maintain and promote everyday skills. For example, Alzheimer’s patients practice dressing, combing, cooking and hanging up laundry.
Other non-drug procedures that are used in Alzheimer’s disease include, for example, art and music therapy, physiotherapy, aromatherapy and “Snoezelen” (stimulation of the senses such as touch, smell, taste, etc.).
Alzheimer’s: course and prognosis

Alzheimer’s disease leads to death after eight to ten years on average. Sometimes the disease progresses much faster, sometimes more slowly – according to the current state of knowledge, the time span ranges from three to twenty years. In general, the later in life the disease occurs, the shorter the course of Alzheimer’s.
Prevent Alzheimer’s
As with many diseases, a healthy lifestyle can reduce the likelihood of getting Alzheimer’s. Factors such as high cholesterol, obesity, high blood pressure and smoking can promote Alzheimer’s and other dementia diseases. Such risk factors should therefore be avoided or treated if possible.
In addition, a Mediterranean diet with lots of fruit, vegetables, fish, olive oil and whole grain bread seems to prevent Alzheimer’s and other forms of dementia.
Regular exercise and sports can also reduce the risk of disease: The reason is that physical activity stimulates the metabolism and blood circulation in the brain, among other things. This allows nerve cells to network better and more densely, which promotes their communication.
The risk of Alzheimer’s and other forms of dementia also decreases if you are mentally active at work and in your free time throughout your life. For example, cultural activities, puzzles, and creative hobbies can stimulate the brain and preserve memory.
As studies have shown, an active social life can also prevent dementia diseases such as Alzheimer’s: the more you socialize and get involved in communities, the greater the likelihood of remaining mentally fit in old age.
