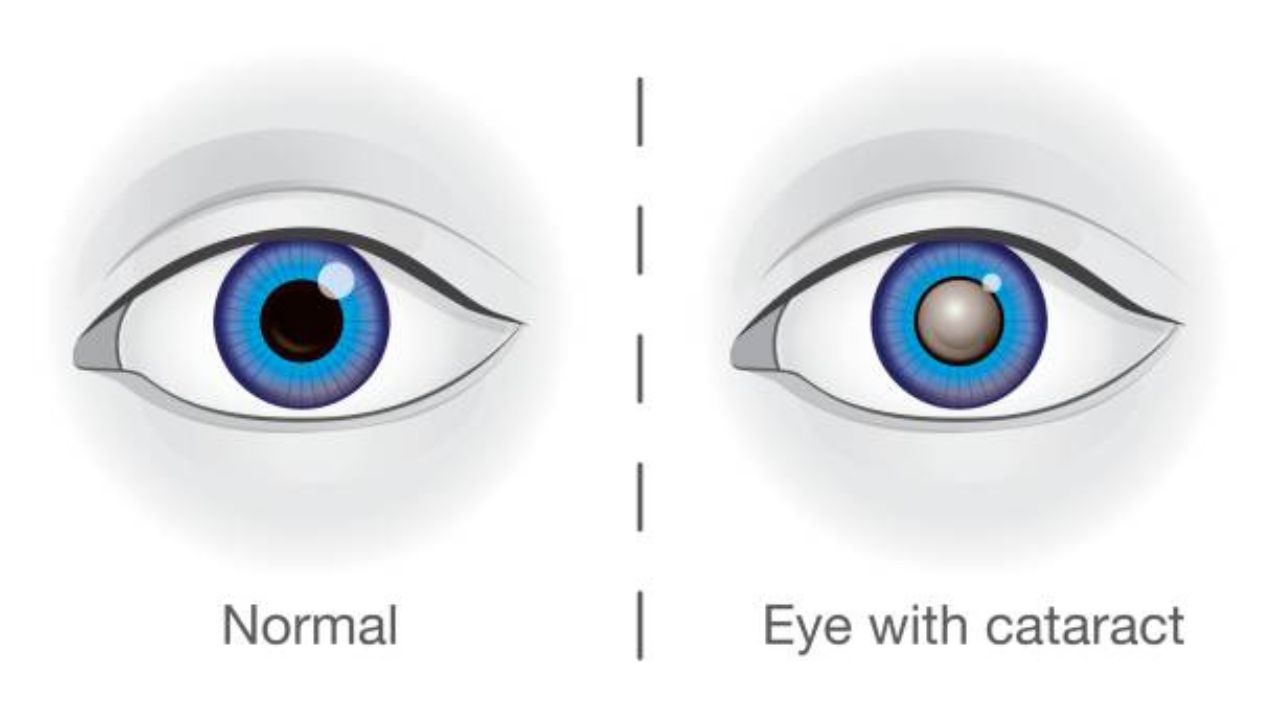
Cataracts are an eye condition that causes the otherwise clear lens to become increasingly cloudy. As a result, the eyesight steadily decreases. Cataracts are often age-related. However, it can also be the result of metabolic diseases or eye malformations and injuries, for example. Cataracts can be treated well with surgery. If left untreated, it can lead to blindness. Read more about cataract symptoms, causes and treatment here!
ICD codes for cataract: H28 | H25 | Q12 | H26
Quick overview
- Symptoms: progressive deterioration of vision, sensitivity to glare, seeing “as if through a haze/fog”.
- Causes: mostly aging processes of the eye, sometimes also other diseases (e.g. diabetes mellitus, eye inflammation), eye injuries, congenital eye malformations, exposure to radiation, heavy smoking, medication.
- Diagnostics: including consultation with the patient, various eye examinations (e.g. using a slit lamp), if necessary further examinations if an underlying disease is suspected (such as diabetes).
- Treatment: surgery.
- Prognosis: generally good chances of success after surgery.
Symptoms of cataract
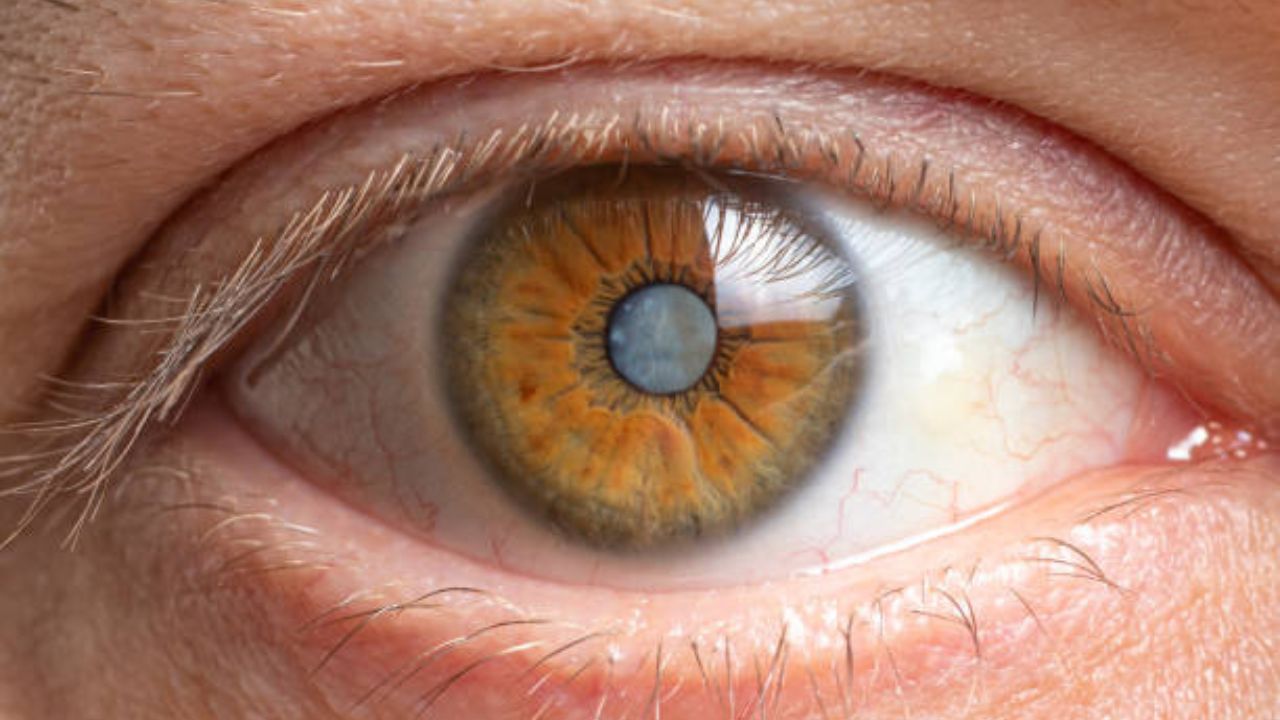
If the view becomes cloudy and the world seems to disappear behind a veil, this could be a sign of the eye disease cataract. “Gray” because the lens turns greyish in advanced disease and thus becomes cloudy. The suffix “Star” derives from the stare that sufferers have when they are (almost) blind due to the eye disease.
The medical term for cataracts comes from the Greek and means “waterfall”. It used to be assumed that coagulated liquid in the eye caused clouding of the lens.
Cataracts: Symptoms in the course of the disease
Depending on the stage, cataracts cause different symptoms. At the beginning of the disease, vision deteriorates and those affected become increasingly sensitive to glare. In the middle of the visual field, a kind of fog is created, through which objects are perceived as blurred or as if they are behind a veil.
This fog becomes denser over time and spreads to cover the entire field of vision as the disease progresses. Colours, contrasts and contours gradually fade and seem to merge with one another. Spatial perception and thus also the ability to orientate deteriorate.
Individual and complete failures of the field of vision, as they occur with glaucoma, do not exist with cataracts.
As the disease progresses, cataracts develop symptoms that can severely burden those affected in everyday life. This includes:
- Significant sensitivity to glare (e.g. in bright sunlight or flashlight).
- Indistinct visual perception.
- Worse light-dark adjustment.
- Straining when reading or watching TV.
- Limited spatial vision.
- Insecurity on the road.
These symptoms can vary in severity in each patient. They do not necessarily (all) have to occur.
Finally, late-stage cataracts make normal everyday life almost impossible: visual performance can deteriorate so dramatically within a short period of time that it is tantamount to blindness.
Cataracts: Symptoms often go unrecognized or misinterpreted for a long time
If cataracts affect both eyes, it is often difficult for those affected to assess how far advanced the visual impairment is. This can be dangerous on the road, for example.
Another problem is that many people with cataracts initially ignore the symptoms, mask them or attribute them to other causes such as fatigue. In the case of cataracts in particular, which occurs as a result of the natural aging process, the symptoms are often attributed to the age-related deterioration of the eyes – and not to a manifest eye disease such as cataracts.
Cataracts: Relatives should watch out for signs
Precisely because those affected often misjudge or deny the deterioration in vision, it is important that the relatives know the symptoms of cataracts and interpret them correctly. In the early stages of the disease, those affected become less confident in their usual activities, such as driving or reading. You can tell that by the fact that the patients often show a strained facial expression during these activities.
In the later stages, the deterioration in vision can become so severe that people often fail to reach for something they are handed or when they want to pick up something themselves. It also takes them a long time to adjust to an environment they are unfamiliar with. Therefore, they often avoid unfamiliar places.
Finding your way around in your own home is also becoming more difficult. People with cataracts usually tend to keep everything in order so that they can find everything even without full vision.
Congenital cataracts: symptoms
Children can also get cataracts. Doctors then speak of childhood or congenital cataracts. The lens opacity can be present at birth or develop over the course of the first few years of life. The first sign of this is often that children start to squint (strabismus).
Parents should not ignore this, but take it seriously. If left untreated, the loss of visual acuity can impair the development of the visual system, which reacts particularly sensitively to disturbances in the first few months of life: If cataracts are not recognized and treated in the baby, a so-called weak sight (amblyopia) can develop.
This weak sight can no longer be corrected at the latest when puberty is reached. Therefore, go to the doctor immediately if signs of cataracts appear in the child!
Cataracts: causes and risk factors
In the vast majority of cases, cataracts are age-related. However, it can also have other causes such as metabolic diseases, other eye diseases or eye injuries.
Natural aging process
The lens of the eye is normally clear and flexible, allowing the small muscles of the eye to deform it as needed. This deformation and the fluid that surrounds the lens allow us to see near and far objects equally sharply. This adaptation of the eye’s refractive power to objects at different distances is called accommodation.
With increasing age, the flexibility of the eye lens naturally decreases, which can result in lens clouding. Therefore, around 90 percent of all cases of cataracts are age-related cataracts. This gray cataract occurs from around the age of 60. According to statistics, almost half of the 52 to 64 year olds have cataracts without even knowing it. Because at the beginning of the disease, there is often no perceptible visual disturbance. From the age of 65 almost everyone has a clouding of the lens of the eye.
Diabetes (diabetes mellitus)
In diabetes mellitus, the sugar content in the eye water (and blood) is increased. Excess sugar (glucose) is stored in the lens, causing it to swell. As a result, the arrangement of the lens fibers shifts and the lens becomes cloudy. Doctors speak of cataracta diabetica here.
In pregnant women with diabetes mellitus, the child in the womb can develop cataracts.
Other metabolic diseases
In addition to diabetes, other metabolic disorders can also promote cataracts. These include, for example:
- Calcium deficiency (hypocalcemia).
- Overactive parathyroid gland (hyperparathyroidism).
- Excess of ferritin in the blood (ferritin is an iron storage protein).
- Galactosemia (an inherited disorder in the utilization of the sugar galactose contained in breast milk).
Eye diseases
A cataract can also be caused by other eye diseases and is then called cataracta complicata. Possible triggers include eye inflammation (such as inflammation of the middle layer of the eye membrane = uveitis) or severe short-sightedness.
Eye injuries
A bruised eyeball from a fist or a tennis ball can cause cataracts, as can a puncture wound or a foreign body that has penetrated deeply into the eye. Such injury-related cases of cataracts are summarized under the technical term cataracta traumatica.
Congenital eye malformations
If cataracts are congenital (cataracta congenita), there can be two reasons:
- Genetic defect: About 25 percent of all congenital cataract diseases are based on a genetic defect that leads to a malformation of the eye and thus to clouding of the lens.
- Infectious diseases during pregnancy: Certain infections in pregnant women (rubella, toxoplasmosis, herpes) can lead to the child being born with a cataract.
Other causes
Defects in the metabolism of the lens, malnutrition, heavy smoking, radioactive radiation and ultraviolet light (UV light) can also trigger cataracts. Drugs or poisoning are very rarely the reason for clouding of the lens.
Cataracts: examinations and diagnosis
A precise examination by the ophthalmologist is necessary for the diagnosis of cataracts.
Medical history
It starts with a detailed discussion between the doctor and the patient to collect the medical history (anamnesis): The doctor asks about the exact symptoms and any underlying diseases (diabetes, eye diseases, etc.).
Eye exams
This is followed by various eye examinations. To do this, the pupil is sometimes dilated first using special eye drops. The following examinations help to diagnose cataracts:
- Brückner test: In this examination, the doctor x-rays the eye. Because the retina reflects part of the light, lens opacities appear as dark spots.
- Slit lamp examination: The slit lamp is a microscope with a light source that can be swiveled to both sides. The bundled, slit-shaped light beam penetrates the transparent eye area. The doctor can also examine the retina at the back of the eye and see what type of cataract is present and what could be the cause.
- Corneal examinations: The doctor can measure the thickness of the cornea (pachymetry) and image its surface and back surface using computer-aided methods (Pentacam). The latter shows whether the cornea is evenly curved and whether the cell layer that supplies the cornea and ensures its transparency is in order (determination of the endothelial cell density).
- General vision test : The ophthalmologist also routinely checks general vision, for example with eye charts, and whether other eye diseases are present.
If cataracts are already well advanced, the clouding of the lens can already be seen with the naked eye.
Other investigations
Sometimes cataracts are the first sign of another underlying condition. Additional examinations, such as skin and muscle tests as well as blood tests, are therefore necessary, especially in young patients. For example, tetany (pathological muscle cramps), myotonia (muscle disease), skin diseases, Wilson’s disease (congenital disorder of copper metabolism) or diabetes mellitus can be diagnosed.
Cataracts: treatment
Cataracts can only be effectively treated by surgery (cataract surgery). The cloudy lens is removed and replaced with an artificial lens. As a rule, the surgeon nowadays no longer removes the entire lens, but leaves the lateral and rear eye capsule in the eye.
Cataract surgery is the most common eye surgery. In Germany alone, the operation is performed around 700,000 times a year, and more than 100 million times worldwide.
The procedure is a so-called microsurgical operation, i.e. it is carried out with an operating microscope. This is possible both in the hospital and in an ophthalmology practice. The artificial lens used remains in the eye for life, so it does not have to be replaced after a while.
Cataract surgery: when is it necessary?
When a cataract is operated on depends on various factors. Doctor and patient jointly determined the time of the operation.
Above all, the subjective perception of the visual impairment plays a role in the decision. If a person affected by the cataract feels severely impaired in everyday life and in professional life, this speaks for an operation.
In other cases, an objective deterioration in vision makes in vision makes the procedure advisable or necessary: people who drive a car have to have an eye test at regular intervals. Above a certain level of visual impairment, it is no longer possible to drive on the road – a good argument for an operation.
In some professions, a certain level of visual acuity is even a mandatory requirement, for example for pilots and professional drivers. Cataract surgery is then often necessary at an early stage of the disease. The subjective perception of the visual performance plays no role here.
If possible, the patient’s fears about the eye surgery are taken into account when deciding for or against an operation. However, if the visual performance has deteriorated to the point of imminent blindness in the case of advanced cataracts , the operation should be carried out despite such fears.
A congenital cataract should be operated on immediately after diagnosis. Only then does the child have the chance to learn to see properly.
Lenses used
The intraocular lens used in cataract surgery is made of plastic. It must have exactly the same refractive power as the removed endogenous lens. The doctor calculates the right lens strength before the procedure by measuring the length of the patient’s eyes with an ultrasound device and determining the refractive power of the cornea.
The artificial lenses used differ in terms of implant location, material and their optical principles.
Differences in implantation site
Depending on the implantation site, a distinction is made between anterior chamber lenses, posterior chamber lenses and iris-supported lenses.
- Anterior chamber lenses (VKL) are inserted into the anterior chamber of the eye (in front of the iris) and fixed there with two brackets in the chamber angle. They are only used for intracapsular cataract extraction (see below) – but only rarely, because anterior chamber lenses can cause glaucoma or clouding of the cornea.
- Posterior chamber lenses (HKL) are inserted into your own capsular bag, which is located behind the iris. If there is no longer a capsular bag, as is the case with intracapsular cataract extraction, the lens is attached to the iris or sclera of the eye with two sutures.
- Iris-worn lenses (iris clip lenses) are attached to the iris with small brackets. Since the cornea is often injured, such lenses are no longer used in Germany. In many cases, iris-supported lenses that have already been implanted are replaced by posterior chamber lenses.
Differences in lens material
In small-incision cataract surgery, silicone or acrylic intraocular lenses are used because these lens materials are foldable. These artificial lenses are inserted into the capsule in a folded state, where they then unfold themselves. They are used exclusively as posterior chamber lenses.
An acrylic lens has a higher refractive index than a silicone lens and is therefore slightly thinner.
Dimensionally stable lenses made of polymethyl methacrylate (PMMA, Plexiglas) can be used both as anterior chamber lenses and as posterior chamber lenses. A slightly larger incision is required for the implantation.
Differences in optical principles
The optical principle refers to the properties of the lens that create the new “sight” in the person affected. Doctors distinguish between monofocal lenses and multifocal lenses.
- Monofocal lens : Like normal glasses, it has only one focal point. It enables sharp vision either at a distance or up close. Before the operation, the patient has to decide whether he would rather live without “distance glasses” after the operation but with reading glasses, or vice versa. The appropriate power of the artificial lenses is selected accordingly.
- Multifocal lens : It offers good visual acuity for both distance and near. Patients will then no longer need glasses for more than 80 percent of their daily tasks. However, multifocal lenses have two disadvantages: contrasts are seen less sharply and the eye becomes more sensitive to glare.
Surgical methods
There are various methods of lens implantation to eliminate lens clouding. Which one is used in individual cases depends on the individual requirements and the stage of the disease.
Intracapsular Cataract Extraction (ICCE)
In this type of cataract surgery, the lens, including the capsule, is removed from the eye. This requires a relatively large incision (eight to ten millimeters) through the cornea. After that, the lens is frozen with a special cold pen and removed from the eye. The surgeon then inserts the artificial lens either in the anterior chamber of the eye (anterior chamber lens) or in the posterior chamber of the eye (posterior chamber lens) and sews up the incision with a fine thread.
Intracapsular cataract extraction is usually only necessary in an advanced stage of the disease.
Extracapsular Cataract Extraction (ECCE)
During extracapsular cataract extraction, the surgeon opens the anterior lens capsule with an incision of about seven millimeters and removes the lens nucleus without crushing it. The artificial lens is now inserted into the intact capsule.
This surgical method is gentle on the cornea. Therefore, it is mainly used when a far advanced cataract has already damaged the thin, innermost layer of the cornea (corneal endothelium).
Phacoemulsification (Phaco)
In phacoemulsification, the cornea is opened with an incision about 3.5 millimeters wide. Then the doctor dissolves the lens nucleus with the help of ultrasound or a laser and sucks it out. The artificial replacement lens is now inserted into the intact shell of the lens (capsule bag): It is folded and pushed through the tiny opening and unfolds itself in the capsular bag. Two semi-circular elastic straps on the edge of the lens ensure a secure hold in the capsular bag.
The tiny incision made during phacoemulsification closes itself after the operation without scars forming. Finally, the surgeon only has to reseal the previously pushed back conjunctiva. Thanks to the small incision, with this surgical method it is possible to fit new glasses earlier than with the others and to resume normal everyday life.
Course of the cataract operation
Cataracts usually appear on both sides. First, however, only one eye is operated on. Once that eye has healed, it’s the turn of the second.
The procedure usually takes less than 30 minutes.
Outpatient procedure, local anesthesia
Cataract surgery is usually performed on an outpatient basis under local anesthesia. The administration of suitable eye drops is usually sufficient for the anesthetic. Alternatively, a local anesthetic can be injected into the skin next to the eye to be operated on. The entire eyeball becomes painless and can no longer be moved. The doctor may also give you a mild sedative before the operation.
Your circulation will be monitored throughout the operation using a blood pressure monitor, oxygen saturation measurement or an ECG.
After the operation, the operated eye is covered with an ointment bandage. You will need to stay in the hospital or doctor’s office for some time to be monitored. If there are no complications, you can go home after just a few hours. In the period that follows, regular check-ups by the doctor treating you are necessary.
What you should consider after the operation
Keep in mind that you are not allowed to drive yourself immediately after cataract surgery. So you should get picked up.
You can have light food and drinks on the day of the operation. You can usually take your usual medication as usual, but you should discuss this with your doctor beforehand. This is especially advisable if you need diabetes medication or blood-thinning medication.
As long as the operated eye is covered with a bandage and the surgical wound has not yet healed, you should take care when showering and washing that the eye does not come into contact with soap.
Physical exertion, swimming, diving, cycling and going to the sauna should be avoided in the initial period after cataract surgery. The same applies to activities that involve a lot of dirt or dust. You can usually read and watch TV again after a week.
You can usually have new glasses fitted four to six weeks after cataract surgery. This does not make sense at an earlier point in time, since the eye first has to get used to the new lens.
If you notice the following symptoms some time after the cataract operation, you should see an ophthalmologist :
- Deterioration of visual acuity
- Increased redness of the eye
- Pain in the eye.
Risks and complications of surgery
About 97 to 99 percent of all cataract surgeries are without complications. However, as with any surgical procedure, there are risks. These include:
Capsule rupture
If the back capsule of the lens ruptures during the operation, complications can arise. The vitreous humor is located behind the lens of the eye. It consists of a gel-like, transparent mass and presses the retina, which is located at the back of the eye, against its base. If the vitreous substance escapes via a lens tear, there is a risk of retinal detachment.
This risk exists in about six to eight percent of intracapsular surgeries; in an extracapsular operation, on the other hand, a capsule rupture hardly ever occurs.
Bacterial infection
Very rarely, during intracapsular cataract surgery, bacteria get inside the eye and cause inflammation (endophthalmitis). This can cause blindness in the affected eye.
Bleeding
During cataract surgery, the pressure in the eye can increase, which can cause blood vessels to burst. The result is bleeding within the eye (intraocular) or within the capsule (intracapsular). However, they are very rare: Such bleeding occurs in less than one percent of all cataract operations.
Corneal curvature
With the extracapsular surgical method, the incision causes a slightly greater curvature of the cornea than before the operation. However, this usually resolves on its own within a few weeks.
“Aftercataract“
Depending on the surgical technique, 20 to 30 percent of patients develop a “secondary cataract” (cataracta secundaria) after a cataract operation: The rear parts of the remaining lens capsule become cloudy. This tends to happen more often in young people than in older people.
With the help of a laser or another surgical procedure (similar to cataract surgery), these clouded parts of the lens can be removed quickly with minimal risk. The eyesight then improves again.
Cataracts: course of the disease and prognosis
If left untreated, cataracts progress slowly but steadily – vision deteriorates until the person becomes blind in the affected eye. This can only be stopped with an operation. The chances of success of the procedure largely depend on the cause of the clouding of the lens:
Age-related cataracts can usually be completely healed by the procedure – most patients regain 50 to 100 percent of their visual acuity.
The surgical result is usually less good in patients whose cataract is caused by another eye disease, such as glaucoma, age-related macular degeneration (AMD) or a diabetes-related retinal disease (diabetic retinopathy). Those affected should discuss with the doctor before the procedure what improvement in visual acuity is likely to be achieved with the procedure.
Even with cataracts due to other causes, the prognosis after the operation is often worse than with age-related cataracts.
Cataracts: prevention
An age-related cataract (senile cataract) cannot be prevented so far – neither by medication nor by other measures such as eye exercises. However, external factors that can trigger cataracts can be very well controlled and avoided.
Protect the eye
For example, you should always wear safety goggles when doing activities that could injure your eyes (such as grinding or drilling).
When out in the sun (especially when skiing), good sunglasses will protect your eyes from dangerous UV rays. You should also wear protective glasses in the solarium.
Attend preventive appointments
From the age of 40, see an eye doctor every 12 to 24 months to have your vision checked. With a regular eye test, cataracts can already be detected when the symptoms are barely pronounced.
If you want to become pregnant, you should check your vaccination protection beforehand and have it refreshed if necessary. This helps prevent infections that can cause cataracts in babies (like rubella).