Cholangitis is inflammation of the bile ducts inside or outside the liver. The typical symptoms of cholangitis are fever, upper abdominal pain and yellowing of the skin. It is a rarer disease that primarily affects women over the age of 40. Cholangitis is most often caused by bacteria or gallstones. It can be treated well with antibiotics or by having a gallstone removed. Here you can read everything you need to know about cholangitis.
ICD codes for this disease: K74 K83 K80
Quick overview
• Symptoms: In acute cholangitis, severe pain in the upper abdomen, often high fever, yellowing of the skin; in the autoimmune forms fatigue, upper abdominal pain, jaundice and severe itching.
• Treatment: In the acute form antibiotics, if necessary removal of gallstones, in the autoimmune forms medication, possibly liver transplantation.
• Causes: In acute cholangitis, a bacterial infection, in the autoimmune forms, narrowing of the bile ducts due to inflammation triggered by the patient’s own immune system.
• Risk factors: Gallstones, narrowing of the bile ducts.
• Diagnosis: Physical examination, blood work, ultrasound and further imaging if necessary.
• Course of the disease: The acute form usually heals with appropriate therapy, the autoimmune forms are lifelong, increased risk of liver cirrhosis and bile duct cancer in PSC.
• Prognosis: Generally good in the acute form, life expectancy often reduced in the autoimmune forms.
What is cholangitis?
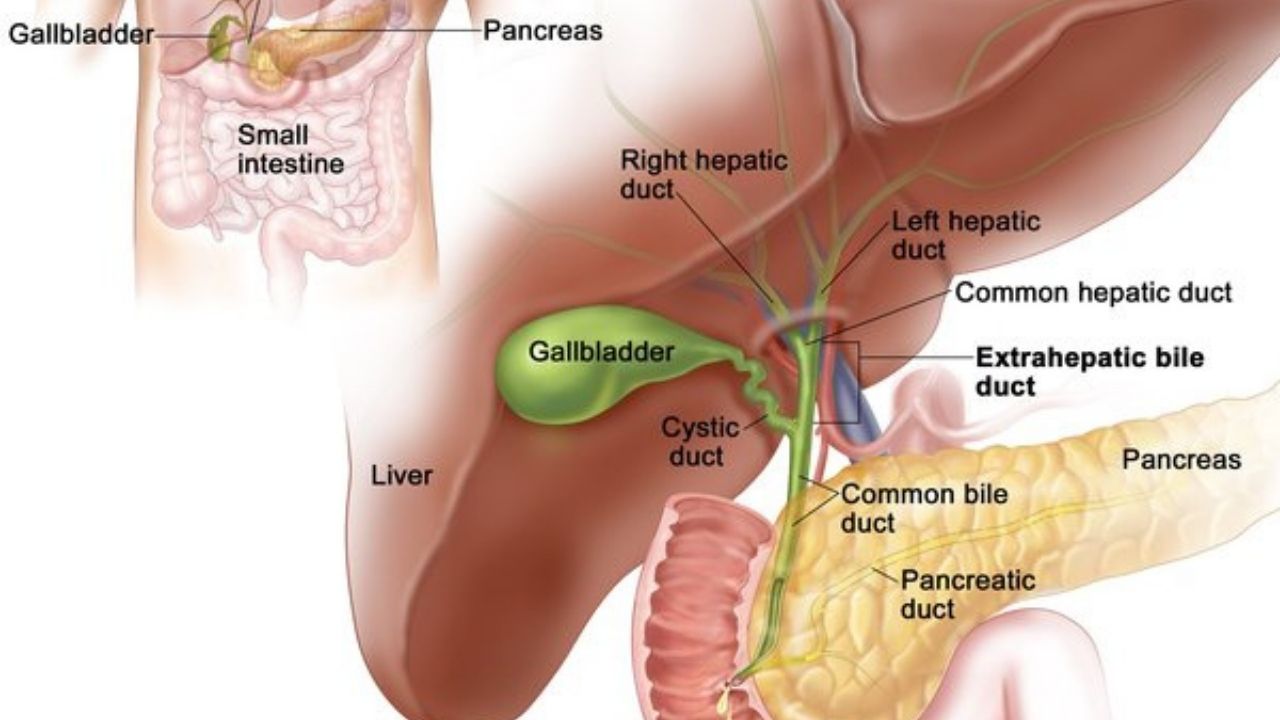
Cholangitis is inflammation of the bile ducts that connect the gallbladder to the small intestine. The bile is produced by the liver cells and concentrated and stored in the gallbladder. When eating, more bile enters the duodenum via the bile ducts. The intestine needs the bile acids it contains in order to break down the fats ingested and make them digestible.
In addition, toxic substances from the body enter the intestine via the liver and bile ducts and are excreted with the stool.
In cholangitis, the bile ducts are inflamed, but the gallbladder is not affected by the inflammation.
Types of cholangitis
Doctors distinguish between an acute bacterial form of cholangitis, which is caused by bacteria ascending from the duodenum, and various special forms that belong to the autoimmune diseases:
Acute bacterial cholangitis
In acute cholangitis, bacteria from the duodenum enter the bile ducts. Under certain circumstances, these settle and trigger an acute, purulent inflammation of the bile ducts. Those affected often suffer from gallstones: These impede the flow of bile and thus promote bacterial colonization. Since overweight women in particular have an increased risk of gallstones from the age of 40, they develop acute cholangitis twice as often as men.
Autoimmune types of cholangitis
In addition to bacterial cholangitis, there are also special forms of bile duct inflammation that are autoimmune diseases:
• Primary biliary cholangitis (PBC) is a nonsuppurative inflammation of the bile ducts within the liver. The cause is unknown, but people with celiac disease have an increased risk of developing the disease. With a share of 90 percent, women are primarily affected, the peak age is around 50 years of age.
• Primary sclerosing cholangitis (PSC) is a chronic progressive inflammation of the bile ducts inside and outside the liver. The disease is closely related to other autoimmune diseases such as the chronic inflammatory bowel disease ulcerative colitis. Men are affected about twice as often as women, mostly between the ages of 30 and 50.
• In contrast to PSC, secondary sclerosing cholangitis (SSC) can almost always have a specific trigger identified, such as poor blood flow in the bile ducts (ischemia), injuries to the bile ducts caused by surgery or certain infections.
The autoimmune forms of cholangitis lead to scarring (sclerotherapy) of the bile ducts and even bile stasis (cholestasis). In the later stages, those affected often develop cirrhosis of the liver, which can only be treated with a liver transplant.
What are the symptoms of cholangitis?
Acute bacterial cholangitis, PBC and PSC show common symptoms as well as some differences in clinical picture. In particular, the symptoms of the autoimmune forms do not develop suddenly, but rather gradually.
Symptoms of acute cholangitis
The typical symptoms of acute cholangitis are severe pain in the upper right abdomen, high fever of over 40 degrees Celsius and a pronounced feeling of illness. Cholangitis also leads to yellowing (icterus) of the skin in many of those affected after a few days. This is caused by the backlog of bile in the liver.
The breakdown product (bilirubin) of the red blood pigment (hemoglobin) is no longer excreted via the bile, enters the blood and is deposited in the skin and mucous membranes. The yellowing of the skin is associated with severe itching in some people.
Symptoms of primary biliary cholangitis
In the early stages, primary biliary cholangitis often causes no or only unspecific symptoms such as chronic tiredness and exhaustion (fatigue) and upper abdominal pain. Many of those affected also complain of massive, excruciating itching.
Because PBC leads to liver fibrosis and cirrhosis as the disease progresses, signs of liver damage such as yellowing of the skin and accumulation of fluid in the abdomen (ascites) later develop. Other symptoms of PBC are lipid metabolism disorders, fatty stools, a lack of fat-soluble vitamins and, especially in women, recurring urinary tract infections.
Symptoms of primary sclerosing cholangitis
PSC often does not cause any symptoms in the early stages. As with PBC, those affected later suffer from yellowing of the skin and excruciating itching. There are also other signs such as unclear upper abdominal pain or weight loss. Since the risk of bacterial inflammation of the bile ducts is increased in PSC, symptoms typical of acute cholangitis are also possible in episodes.
How is cholangitis treated?
Therapy for cholangitis depends on the cause of the disease.
Bacterial cholangitis
Acute bile duct inflammation is usually triggered by bacteria. The doctor therefore usually prescribes high-dose antibiotics for the affected person. In some cases, he also uses a combination of two different classes of antibiotics with different mechanisms of action in order to cover a larger spectrum of germs (broad-spectrum antibiotics).
People with acute cholangitis are advised not to eat for at least 24 hours to prevent bile flow. In addition, those affected receive painkillers such as metamizol and antipyretics such as paracetamol and ibuprofen. The pain usually subsides after a few days. It is also recommended that those affected drink enough fluids.
Gallstone removal
If the cholangitis is due to blockage of the bile ducts by gallstones, it is important to remove them. Under certain circumstances, the surgeon inserts a so-called stent in the bile duct. The stent is a tube that keeps the bile duct open, improving the flow of bile into the small intestine.
Gallstones form mainly in the gallbladder and from there migrate into the bile duct system. After an acute flare-up of inflammation, the gallbladder is usually surgically removed (cholecystectomy).
Primary sclerosing cholangitis
The primary sclerosing cholangitis and the primary biliary cholangitis are autoimmune diseases and up to now cannot be treated causally. Since those affected often suffer from jaundice, the drug-based excretion of bile acids is the main therapeutic focus. The drug ursodeoxycholic acid not only improves jaundice, but also improves the prognosis of those affected, at least in the case of PBC.
In acute episodes of inflammation in the context of PSC, the doctor also uses antibiotics. If there is a lack of fat-soluble vitamins, those affected receive appropriate vitamin preparations to counteract deficiency symptoms.
In the course of the disease, PSC and PBC lead to progressive scarring of the liver tissue (liver cirrhosis). In the final stage of liver cirrhosis, the last treatment option is a liver transplant.
Causes and risk factors
Acute cholangitis and the autoimmune forms PBC and PSC have very different causes.
Acute cholangitis caused by intestinal bacteria
Acute cholangitis is often caused by intestinal bacteria that migrate from the small intestine via the main bile duct (ductus choledochus) into the gallbladder and the bile duct system. The main bile duct, together with the excretory duct of the pancreas (ductus pancreaticus), opens into the duodenum (duodenum).
A sphincter regulates the opening of the common duct. Although the sphincter usually prevents intestinal bacteria from ascending to the liver, occasionally bacteria can enter the bile ducts, possibly leading to cholangitis.
Acute cholangitis caused by gallstones
Gallstones are usually caused by high levels of cholesterol in the bile. Overweight women over the age of 40 are particularly at risk and often have gallstones.
If the gallstones migrate from the gallbladder into the bile duct system, they block the bile ducts, causing the bile secretion to back up – sometimes as far as the liver. Bacteria in the bile ducts multiply more easily under these conditions. The bile duct mucosa is then irritated and purulent inflammation (cholangitis) spreads more quickly.
A narrowing of the bile ducts, for example due to anatomical peculiarities, a tumor or surgical interventions in the area of the bile ducts, increases the risk of cholangitis.
PSC and PBC: autoimmune diseases
Primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC) are special forms of cholangitis that are based on an autoimmune inflammatory process. The bile ducts of those affected are chronically inflamed and narrow as the disease progresses, leading to a backlog of bile. The reason why the immune system attacks the body’s own tissues is not known.
Investigations and diagnosis
The right contact person if cholangitis is suspected is a specialist in internal medicine or gastrointestinal diseases (gastroenterology). The doctor asks the person concerned about the current symptoms and asks them to describe the symptoms and any previous illnesses (anamnesis). The localization, type and duration of the pain, abnormalities during bowel movements and accompanying symptoms provide important indications of cholangitis.
The physical examination is then carried out, during which the doctor takes a closer look at the skin, among other things, if cholangitis is suspected. Any yellowing of the skin or so-called liver skin signs indicate liver damage. Liver skin signs are typical skin changes that occur in chronic liver diseases. These include, for example, star-shaped enlargements of skin vessels (spider naevi), reddening of the palms of the hands (palmar erythema) and very red, smooth, lacquer-like shiny lips.
The doctor also listens to the abdomen with a stethoscope to check the bowel sounds and the air and stool levels in the bowel. He also feels his stomach. The doctor often presses under the right costal arch and asks the person concerned to take a deep breath. If the pain increases and the affected person stops breathing reflexively, the suspicion of an inflammation is strengthened. During the palpation, the doctor also examines the liver and spleen, which are often enlarged in PBC.
Since cholangitis can only be partially detected by physical examination, further examinations usually follow:
Blood test
In the case of cholangitis, signs of inflammation can be detected with the help of a blood test. Increased values for the so-called C-reactive protein (CRP) and the white blood cells (leukocytes) indicate a bacterial inflammation. However, these inflammatory parameters in the blood are not specific to cholangitis, but also occur as part of other inflammatory reactions.
In the case of PBC and PSC, the so-called cholestasis parameters are often elevated. These are laboratory values that indicate bile stasis, for example total bilirubin and alkaline phosphatase (AP). In PBC, increased liver and cholesterol levels (hypercholesterolemia) may occur later in the disease course.
Since PBC is an autoimmune disease, the concentration of specific autoantibodies (AMA-M2 and PBC-specific ANA) is also increased. These are antibodies that specifically target the body’s own structures. Specific PSC auto-antibodies, on the other hand, are not known, but the so-called ANCA, the antineutrophil cytoplasmic antibodies, are elevated in many of those affected.
Ultrasound
The ultrasound examination of the abdomen (abdominal sonography) may provide initial indications of the cause of cholangitis. Dilated bile ducts indicate a bile congestion. If there are gallstones in the bile duct system, they usually form in the gallbladder and are best visualized there.
More imaging
If primary sclerosing cholangitis is suspected, magnetic resonance cholangiopancreatography (MRCP) is considered a reliable diagnostic tool; in some cases, endoscopic retrograde cholangiopancreatography (ERCP) is also used.
In contrast to ERCP, MRCP is non-invasive. The depiction of the bile ducts is carried out with the help of magnetic resonance tomography.
The ERCP allows imaging of the bile ducts from the inside. The doctor pushes a thin tube through the esophagus and stomach into the duodenum, through which he injects X-ray contrast medium into the common duct of bile and pancreas. He then uses an X-ray machine to examine the bile duct system. If gallstones can be detected, they will be removed directly during the examination.
Course of the disease and prognosis
If the acute cholangitis heals and the doctor removes any gallstones, the prognosis for bile duct inflammation is very good. For most of those affected, it remains as a one-time illness.
In the case of acute bacterial cholangitis, treatment with antibiotics is very important so that the bacteria do not spread throughout the body via the bloodstream and lead to blood poisoning (cholangiosepsis). In advanced stages, bile duct inflammation may spread to the remaining liver tissue and cause purulent abscesses.
The longer the cholangitis persists, the greater the risk of narrowing (strictures) and scarring of the bile ducts. Narrowing of the bile ducts prevent unrestricted drainage of bile and increase the risk of bile congestion.
The autoimmune forms of cholangitis PSC and PBC cannot be cured. They are also associated with an increased risk of liver cirrhosis, and the PSC is also associated with an increased risk of bile duct cancer (cholangiocellular carcinoma).
While acute cholangitis is not associated with a reduction in life expectancy, life expectancy is reduced in PSC and PBC. The five-year survival rate for people with symptomatic PBC is about 50 percent (it is 90 percent for those affected without symptoms). The median survival time for PSC without a liver transplant is about 10 to 20 years from the time of diagnosis.
