COPD ICD 10 (Chronic obstructive pulmonary disease) is a progressive, life-threatening lung disease characterized by inflammation of the airways and obstruction (edema) of the bronchi. This disease is not always easy to diagnose, which increases its danger.
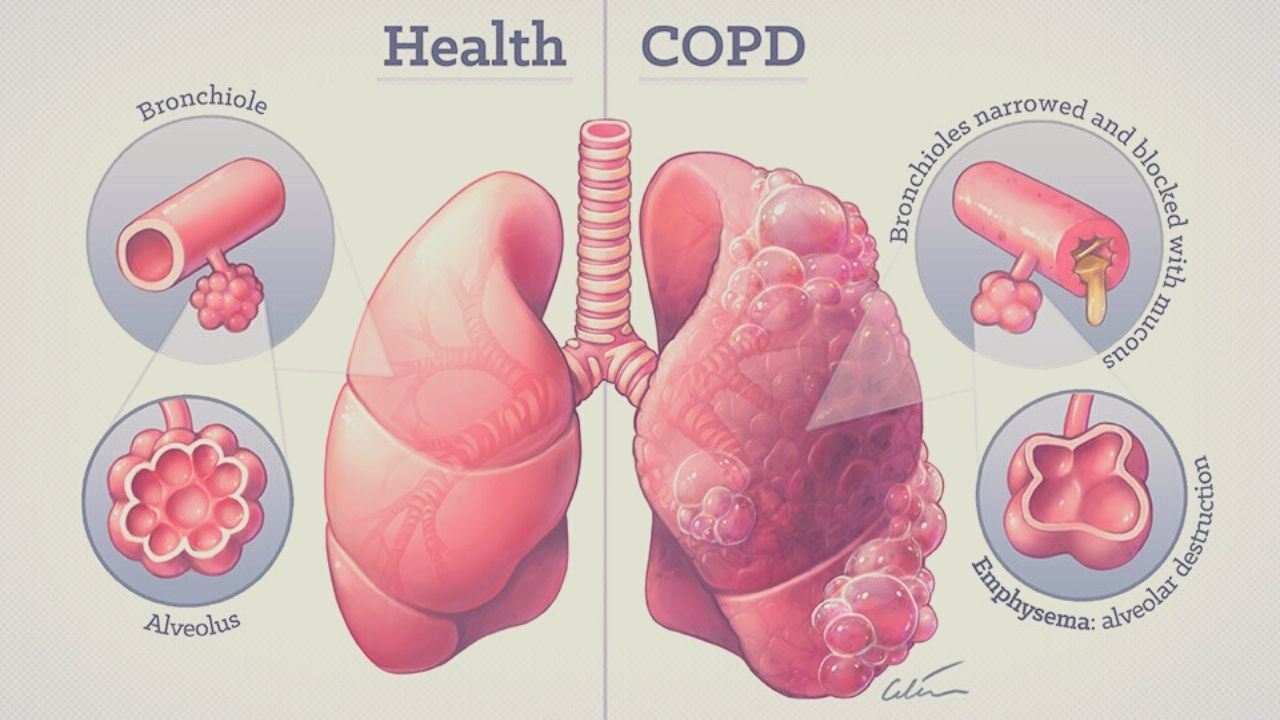
The criterion for COPD ICD 10 is chronic inflammation that affects the central airways, peripheral airways, the lung parenchyma, alveoli, and the vasculature of the lungs.
Disease COPD ICD 10
classification International classification of diseases 10th revision
Chronic obstructive pulmonary disease (J44):
J44.0 – Chronic obstructive pulmonary disease with acute lower respiratory tract infection.
J44.1 – Unspecified chronic obstructive pulmonary disease with exacerbation.
J44.8 – Other specified chronic obstructive pulmonary disease. Chronic bronchitis: asthmatic (obstructive), emphysematous.
J44.9 – Unspecified chronic obstructive pulmonary disease.
In 2011, a classification was proposed , developed by an international group of experts GOLD and based on an integral assessment of the severity of COPD:
A – low risk of exacerbations, symptoms are not expressed;
B – low risk of exacerbations, symptoms are pronounced;
C – high risk of exacerbations, symptoms are not expressed;
D – high risk of exacerbations, symptoms are pronounced.
COPD includes:
- Chronic obstructive bronchitis, in which a patient has a wet (productive) cough that is not caused by other diseases for three months or more.
- Emphysema is a pathological expansion of internal cavities (in this case, the lungs), in which tissues are unnaturally stretched and swollen. A so-called valve mechanism arises – air easily penetrates into tissues, but comes out with difficulty. Obliteration of the small airways is thought to be the primary injury preceding the development of emphysema.
The main components of these changes are the narrowing and remodeling of the airways, an increase in the number of goblet cells, an increase in the mucus-producing glands in the central airways, and, finally, subsequent changes in the vascular bed. Enlarged alveolar spaces sometimes coalesce into bullae (air cysts), defined as air spaces ≥ 1 cm in diameter. These changes lead to a loss of elasticity of the lung tissue and the development of hyperactivity.
Symptoms of COPD ICD 10
The main symptoms of chronic obstructive pulmonary disease (COPD ICD 10) include:
- shortness of breath, or a feeling of lack of air – at first with physical exertion, and subsequently at rest; shortness of breath increases in a dusty space, in the cold, in the presence of irritating substances in the air;
- chronic cough with or without phlegm;
- lengthening the expiratory phase with calm and especially with forced breathing;
- wheezing;
- barrel chest (anterior-posterior chest size increases).
COPD ICD 10 progression is manifested by an increase in coughing and an increase in the amount of sputum, which may be purulent. In the future, difficulty breathing occurs even when performing simple actions – walking or dressing. At the same time, patients begin to lose weight, feel inexplicable weakness, they develop cyanosis (blueness) of the skin, signs of heart failure increase, swelling of the legs occurs, fluid can accumulate in the abdominal cavity (ascites), and the liver enlarges.
Exacerbations can lead to a marked decrease in working capacity and the need for emergency medical care (including hospitalization).
Causes of COPD ICD 10
The main cause of COPD ICD 10 is airflow restriction caused by the inflammatory response to inhaled toxins, most commonly tobacco smoke, including secondhand smoke.
Among other reasons for the development of the disease are unfavorable environmental conditions (air pollution by industrial waste, exhaust gases, smoke, dust, etc.), professional activities (work in mines, chemical plants, in hot workshops), climatic conditions (high humidity), infectious agents (mycoplasmas, pneumococci, Haemophilus influenzae, influenza viruses, adenoviruses, etc.).
Risk factors for the development of COPD ICD 10
Risk factors for the development of COPD ICD 10 include alpha-1-antitrypsin deficiency, high levels of IgE immunoglobulin, familial nature of the disease, genetic predisposition (blood group A (II), lack of IgA).
COPD ICD 10 takes years to develop. Typically, the first symptom is a productive cough that develops in smokers between the ages of 40-50. Most patients have been smoking more than 20 cigarettes / day for more than 20 years. Exacerbations and comorbid conditions are an integral part of the disease and make a significant contribution to the clinical picture and prognosis. As COPD progresses, exacerbations of the disease become more frequent, averaging 1-3 episodes per year. Since COPD is a progressive disease, complete normalization of lung function is impossible.
Diagnosis of COPD ICD 10
Disease can be suspected based on history, physical examination, and x-ray. The diagnosis is confirmed by functional breathing tests. The most important diagnostic method is spirometry, where the vital capacity of the lungs, the forced expiratory volume in 1 second and other indicators are measured according to a certain scheme.
In addition to spirometry, a comprehensive study of the function of external respiration includes a diffusion test, a test with a bronchodilator drug, and bodyplethysmography.
Cytological examination of sputum allows you to assess the nature of inflammation in the bronchi and lungs, to identify the presence of bacteria and viruses.
Sputum examination
A cytological examination of sputum is carried out to establish the nature of the pathological process taking place in the lungs, including with suspicion of tuberculosis and lung cancer.
Pulse oximetry
Pulse oximetry (determination of blood oxygen saturation) is used for all patients with clinical signs of respiratory failure.
If the oxygen saturation of the arterial peripheral blood is less than 92%, then a blood gas analysis must be taken.
Lungs x-ray
X-rays of the lungs can rule out other diseases of the respiratory system. Usually, in patients with COPD ICD 10 on the radiograph, compaction and deformation of the bronchial walls, emphysematous changes in the lung tissue are determined. CT scans of the chest provide better visualization of the type and distribution of lung tissue damage and the formation of bullae than x-rays.
Plain chest x-ray
X-ray examination of the lung structure in order to diagnose various pathologies.
For shortness of breath, a 6-minute walk test is prescribed. Signs of right ventricular hypertrophy, pulmonary heart disease, arrhythmia, ischemia are determined using electrocardiography and echocardiography. With absolute indications, bronchoscopy is performed.
ECG
The study of the functional capabilities of the heart is fast, painless and informative.
Echocardiography
A study to assess functional and organic changes in the heart, its contractility, as well as the state of the valve apparatus.
CBC
A complete CBC is done to assess the severity of an exacerbation of COPD and may detect polycythemia (hematocrit> 55%), anemia, and leukocytosis.
Which doctors to contact
At the first stage, until the diagnosis is established, you should make an appointment with a general practitioner or general practitioner.
Pulmonologists treat COPD ICD 10 . To select the most effective therapy, you may need to examine and consult a cardiologist and other specialized specialists.
The most important goal of COPD ICD 10 treatment is to maintain the patient’s ability to live a normal life and stay active longer. Regardless of the severity of the disease, it is extremely important to reduce the risk of exacerbations and progression of the disease:
- reducing exposure to risk factors, including smoking and air pollution;
- the use of bronchodilators (bronchodilators) – the main drugs in the symptomatic treatment of COPD ICD 10, which are prescribed one-time or regularly;
- the use of inhalations with glucocorticosteroids, which have anti-inflammatory activity;
- the use of a phosphodiesterase-4 inhibitor, the action of which is aimed at suppressing specific inflammation in COPD ICD 10;
- the use of mucolytics that thin the phlegm;
- antibiotic therapy;
- the use of anticholinergics to reduce the reaction of the bronchi to external stimuli;
- supportive therapy (physiotherapy, pulmonary rehabilitation);
- oxygen therapy to relieve respiratory distress – non-invasive / invasive mechanical ventilation.
Chronic symptoms of COPD ICD 10 are treated with short-acting beta-agonists, and exacerbation with inhaled corticosteroids, long-acting beta-agonists, long-acting anticholinergics, or combinations thereof.
During exacerbations, patients with concomitant bronchiectasis may require more intense and longer antibiotic therapy.
Surgical procedures (removal of bullae, lung volume reduction surgery, and lung transplantation) are the final steps in the treatment of COPD ICD 10. Endobronchial valve placement or thermal ablation can lead to clinically significant improvement in a specific group of patients. Patients with terminal phase of COPD are provided with palliative care, the goal of which is to improve the quality of life and daily functioning.
Complications of COPD ICD 10
Along with airflow restriction and respiratory failure, COPD ICD 10 can cause the following complications:
- emphysema of the lungs;
- bronchiectasis;
- respiratory failure;
- pulmonary heart;
- pulmonary embolism;
- cardiac arrhythmias: polymorphic atrial tachycardia, atrial fibrillation.
Other concomitant or complicating pathologies that interfere with the quality of life of patients and affect survival are osteoporosis, depression, anxiety disorders, coronary heart disease, lung cancer and other cancers, muscle atrophy, and gastroesophageal reflux. The extent to which these disorders are associated with COPD ICD 10, smoking, and concomitant systemic inflammation remains unclear.
The main causes of death are acute respiratory failure, pneumonia, lung cancer, heart disease, or pulmonary embolism. Obstructive sleep apnea, which is often found in patients with COPD ICD 10, is associated with an increased risk of hospitalization and death in this group of patients.
The relevance of the problem of the comorbidity of the new coronavirus infection COVID-19 and chronic obstructive pulmonary disease is due to the similarity of clinical manifestations, the complexity of diagnosis, the potential severity of the course and the mutual aggravation of these pathologies.
COPD ICD 10 patients infected with SARS-CoV-2 represent a vulnerable group of people with a complicated course and often poor outcome of the disease.
Prevention of COPD ICD 10
Identifying risk factors and addressing them is the most important step in preventing COPD .
These include:
- motivation to quit smoking;
- elimination of the effects of secondhand smoke;
- reducing exposure to indoor air pollution.
If the work involves the inhalation of harmful substances, it is necessary to use personal protective equipment (respirators).
In case of unfavorable environmental conditions in the place of permanent residence, it is useful to install air purifiers, ionizers, humidifiers in the apartment.
For patients with COPD ICD 10, in order to reduce the risk of exacerbations, vaccination against influenza and pneumococcal infection is recommended. those suffering from COPD ICD 10.
Treatment for COPD ICD 10
Treatment of COPD ICD 10 includes measures such as
- Oxygen support
- Bronchodilators
- Corticosteroids
- Antibiotics
- Sometimes mechanical ventilation with non-invasive ventilation or intubation and ventilation
The immediate immediate goal of therapy is to ensure adequate oxygenation and normalization of blood pH, eliminate airway obstruction and influence the causes.
The causes of an exacerbation usually go unrecognized, although some exacerbations are caused by bacterial or viral infections. Smoking, inhalation of inhalation irritants and high levels of air pollution can also contribute to the development of an exacerbation.
Mild exacerbations can be treated on an outpatient basis with adequate home conditions. Elderly frail patients and patients with concomitant diseases, a history of respiratory failure or acute blood gas disorders should be referred to hospital for observation and treatment. Patients with life-threatening disorders, manifested by uncorrectable moderate or severe hypoxemia, acute respiratory acidosis, the appearance of new arrhythmias or deteriorating lung function, despite being treated in a hospital, should be referred to the intensive care unit, where there is the possibility of frequent monitoring of respiratory status.
Oxygen support for exacerbation of COPD ICD 10
Many patients need oxygen support during an exacerbation of COPD, and even those who do not need it all the time. Hypercapnia may increase with oxygen administration. Usually this increase is considered a consequence of the weakening of the hypoxic activation of the respiratory center. However, an increase in ventilation-perfusion ratio (V / Q) mismatch is probably a more important factor.
Before the appointment of oxygen therapy, the V / Q ratio decreases with vasoconstriction of the pulmonary vessels due to a decrease in perfusion in poorly ventilated areas of the lungs. An increase in V / Q mismatch arises from a decrease in hypoxic pulmonary vasoconstriction when oxygen is administered.
Hypercapnia may be enhanced by the Haldane effect, but this version is questionable. The Haldane effect is to reduce the affinity of hemoglobin to carbon dioxide, which leads to an excessive accumulation of carbon dioxide dissolved in the blood plasma. Oxygen therapy is recommended even though it may worsen hypercapnia; many patients with COPD ICD 10 may have both chronic and acute hypercapnia, and therefore severe central nervous system depression is unlikely if PaCO2 > 85 mm Hg. The target level for PaO2 is about 60 mm Hg; higher levels have little effect, but increase the risk of hypercapnia.
For patients prone to hypercapnia (for example, an elevated serum bicarbonate level may indicate compensated respiratory acidosis), oxygen is administered via nasal cannulas or a venturi mask so that oxygen supply can be carefully controlled and the patient’s condition closely monitored. Patients whose condition worsens with oxygen therapy (for example, patients with severe acidemia or central nervous system damage) require additional ventilation.
Many patients who first needed oxygen therapy at home after being discharged from the hospital, where they were in connection with an exacerbation of COPD ICD 10, improved within 30 days, and they no longer needed further oxygen. Therefore, the need for home oxygen therapy should be reassessed 60–90 days after discharge.
Ventilation support
Non-invasive supply and exhaust ventilation (eg, pressure support or dual supply and exhaust ventilation with a face mask) is an alternative to full mechanical ventilation. Non-invasive ventilation appears to reduce the need for intubation, reduce hospital time, and reduce mortality in patients with severe exacerbations (defined as pH < 7.30 in hemodynamically stable patients without the threat of respiratory arrest).
In patients with less severe exacerbations, non-invasive ventilation is ineffective. However, it can be used in patients with milder exacerbations but whose blood gas is deteriorating despite medication and oxygen therapy, or for those who are likely to require mechanical ventilation but do not need intubation to control the airway or sedation to relieve arousal. In severe shortness of breath, increased airiness of the lungs and against the background of involvement of additional respiratory muscles, artificial ventilation of the lungs with positive pressure can also alleviate the patient’s condition. Deterioration in the presence of non-invasive ventilation will lead to a transition to full mechanical ventilation.
Deteriorating blood gas readings, deteriorating mental status, and progressive depletion of the respiratory muscles are indications for endotracheal intubation and mechanical ventilation. Ventilator setup, ventilation control strategies, and procedure complications are discussed elsewhere. Risk factors for the development of ventilatory dependence are: FEV1 < 0.5 L, stable blood gas composition with PaO2 < 50 mm Hg. or PaCO2 >60 mm Hg, significant limitation of physical activity and severe violations of nutritional status. However, consent from high-risk patients for intubation and mechanical ventilation should be obtained and documented as long as their condition is stable and they are followed up on an outpatient basis. However, addressing the possible need for ventilation should not delay the management of acute respiratory failure; many patients who require mechanical ventilation of the lungs may return to their original state before the exacerbation.
Also, the method of nasal high-flow oxygen therapy was tested in patients with acute respiratory failure on the background of exacerbation of COPD ICD 10 and can be used in those who cannot tolerate non-invasive ventilation with a mask.
For patients requiring prolonged intubation (for example, more than 2 weeks), a tracheostomy is indicated to increase comfort, facilitate communication and facilitate food intake. With a good multidisciplinary pulmonary rehabilitation program that includes adequate nutrition and psychological support, many patients who have required prolonged mechanical ventilation can successfully manage without it and return to their previous functional status. Specialized programs are available for patients who remain ventilator-dependent after acute respiratory failure. In some patients, the ventilator can be turned off for the whole day. Educating family members of patients with adequate home care may allow some patients to go home with a ventilator.
| Dealing with the possible need for ventilation should not delay the treatment of acute respiratory failure; many patients who require mechanical ventilation of the lungs may return to their original state before the exacerbation. |
Drug therapy for exacerbation of COPD ICD 10
Together with oxygen therapy (regardless of the form in which oxygen is prescribed), in order to eliminate airway obstruction, treatment with beta-agonists and anticholinergic drugs with or without the addition of corticosteroids should be started. Methylxanthines, previously considered essential in the treatment of exacerbations of COPD ICD 10, are no longer used; their toxicity exceeds their beneficial effect.
Beta agonists
Short-acting beta-adrenergic agonists form the basis of drug therapy for exacerbations of COPD. The most common drug is albuterol 2.5 mg via a nebulizer or 2–4 sprays (100 mcg / inhalation) from a metered-dose inhaler every 2–6 hours. Inhalation through a metered-dose inhaler provides rapid bronchodilation: there is no evidence that the administration of the drug through a nebulizer is more effective than the correct administration of the same doses of the drug from a metered-dose inhaler. In cases of severe, treatment-resistant bronchospasm, long-term nebulizer therapy can be used.
Anticholinergic drugs
Ipratropium, an anticholinergic drug, is effective for exacerbations of COPD ICD 10 and can be given with or alternately with beta-agonists. The dosage is 0.25–0.5 mg via a nebulizer or 2–4 sprays (17–18 mcg of medication delivered by injection) from a metered-dose inhaler every 4–6 hours. Ipratropium usually has a bronchodilating effect similar to that which occurs when using the recommended doses of beta-adrenergic agonists.
The role of long-acting anticholinergic drugs in the treatment of exacerbations is not fully understood.
Corticosteroids
Corticosteroids should be prescribed immediately for all, even mild, exacerbations. Treatment options include prednisone 30–60 mg orally once daily for 5 to 7 days, with immediate discontinuation or tapering over 7–14 days, depending on clinical response. The oral alternative is methylprednisolone 60–500 mg IV 1 time per day for 3 days, followed by a gradual dose reduction over 7–14 days. These drugs are equivalent in their immediate effect.
Antibiotics
Antibiotics are recommended for exacerbated patients with purulent sputum. Some doctors prescribe antibiotics empirically for sputum discoloration or nonspecific changes on a chest x-ray. Cultures and Gram staining prior to treatment should not be performed unless an atypical or resistant microorganism is suspected (for example, in hospitalized or immunocompromised patients). Medicines aimed at eliminating the microflora of the oral cavity are indicated. Examples of antibiotics that are effective:
- Trimethoprim / sulfamethoxazole 160 mg / 800 mg orally twice a day
- Amoxicillin 250 to 500 mg orally three times a day
- Doxycycline 50-100 mg orally 2 times a day
- Azithromycin 500 mg orally once a day
The choice of drug is dictated by the local antibacterial resistance and the patient’s medical history. Trimethoprim / sulfamethoxazole, amoxicillin, and doxycycline are prescribed for 7-14 days. An alternative first-line antibiotic is azithromycin 500 mg orally once a day for 3 days or 500 mg orally once on the first day, then 250 mg once a day from days 2 to 5.
If the patient is critically ill or there is clinical evidence that infectious agents are resistant, then broad spectrum 2nd generation drugs should be used. These drugs are amoxicillin / clavulanate 250–500 mg orally 3 times daily, fluoroquinolones (eg, ciprofloxacin, levofloxacin), and second-generation cephalosporins (eg, cefuroxime, cefaclor). These drugs are effective against the beta-lactamase-producing strains of Haemophilus influenzae and Moraxella catarrhalis , but they have not been shown to be more effective than the first-line drugs prescribed for most patients.
Patients need to be explained that a change in sputum color from normal to purulent is a sign of an exacerbation and that it is necessary to undergo a 10-14 day course of antibiotic therapy. Long-term antibiotic prophylaxis is only recommended for patients with structural changes in the lungs such as bronchiectasis or infected bullae. In patients with frequent exacerbations, long-term use of macrolides reduces the frequency of exacerbations, but may be accompanied by undesirable effects.
Other drugs
Antitussives such as dextromethorphan and benzonatate are not essential.
Opioids (eg, codeine, hydrocodone, oxycodone) are useful for relieving symptoms (eg, severe coughing fits, pain) given that these drugs can suppress productive coughs, worsen mental status, and cause constipation.
Palliative care for exacerbation of COPD ICD 10
In patients with severe stages of the disease, physical activity is undesirable and daily activity is aimed at minimizing energy costs. For example, patients can limit their living space to one floor of the house, eat more often and in small portions, rather than rarely and in large quantities, and avoid tight shoes. Care for the incurable patient should be discussed , including the inevitability of mechanical ventilation, the use of temporarily pain relieving sedatives, and the appointment of a medical decision maker if the patient is disabled.
Key points for treating acute exacerbation of COPD ICD 10
- Most patients with an exacerbation of chronic obstructive pulmonary disease (COPD) require additional oxygen support during an exacerbation.
- Short-acting beta-agonists form the basis of drug therapy for acute attacks of the disease.
- With exacerbations and separation of purulent sputum, antibiotics are prescribed.
- At the terminal stage of COPD, measures are actively carried out to care for terminal patients, taking into account the patient’s preferences regarding mechanical ventilation and palliative sedation.