Chronic obstructive pulmonary disease or COPD refers to respiratory (lung) disease that obstructs the airways in the lungs and causes breathing problems. Chronic bronchitis (inflammation of the airways or bronchial tubes) and emphysema (damage to the lining of the air sacs in the lungs) are usually part of this condition. You can find out everything you need to know about the causes, symptoms, diagnosis and COPD medicine here.
Your doctor may perform lung (pulmonary) function tests, also called spirometry, or arterial blood gas analysis to help diagnose this condition. A chest X-ray or CT scan of the chest may be used to measure the extent of your disease. Although there is no cure for COPD, your doctor may recommend lifestyle changes, therapies, COPD medicines, and/or surgery to help relieve symptoms.
What is chronic obstructive pulmonary disease (COPD)?
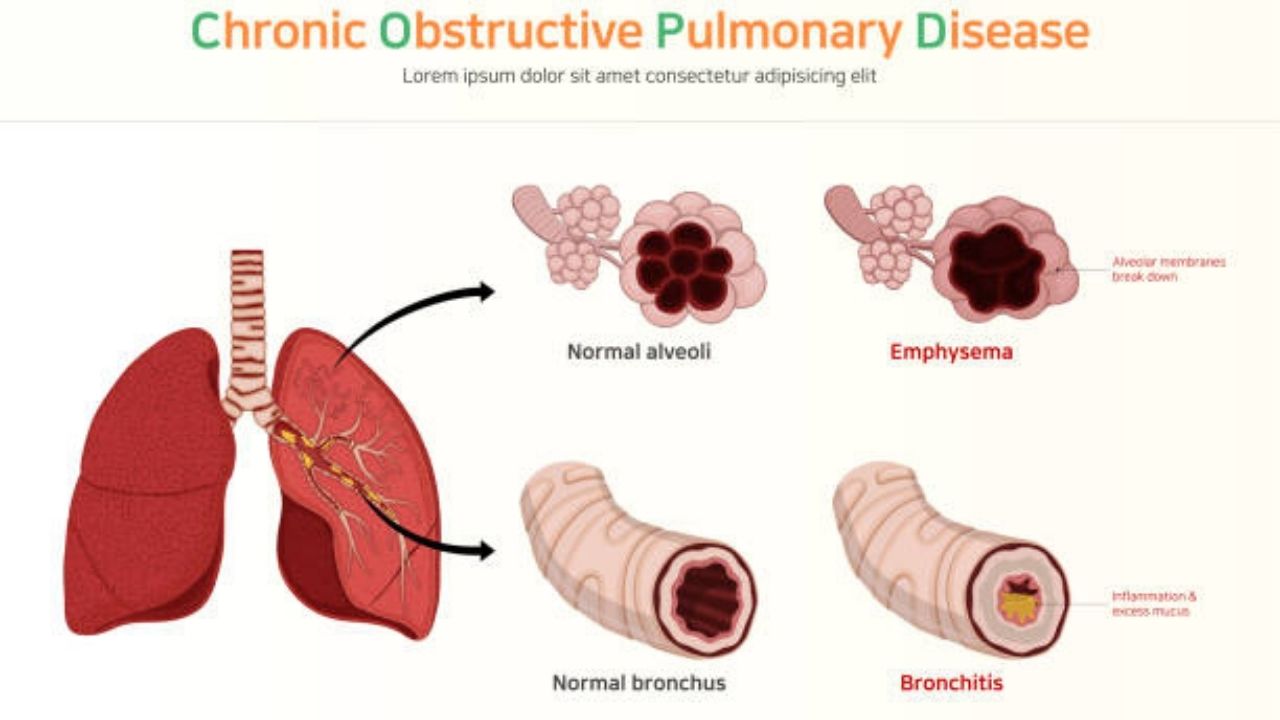
Chronic obstructive pulmonary disease (COPD) refers to lung diseases that obstruct the flow of air from the lungs and cause breathing difficulties. Chronic bronchitis and emphysema are usually part of this condition.
Chronic bronchitis is inflammation of the airways or bronchial tubes. This swelling can cause narrowing and excess mucus, blocking airflow. You may develop a long-standing cough that is produced in order to remove mucus from the airways. For bronchitis to be considered chronic, you must have a cough that lasts for at least three months per year, over a two-year period.
Emphysema occurs when the lining of the air sacs has been damaged and holes form in the lungs. Once air is trapped in these holes, the lungs slowly increase in size and lose their elasticity. This makes it more difficult to breathe because the lungs cannot fully exhale.
Symptoms of chronic obstructive pulmonary disease?
Symptoms of COPD can include:
- Shortness of breath, especially during physical activity
- Chronic cough, usually with excess mucus
- Recurrent respiratory infections
- Wheezing
- Sensation of pressure in the chest
- Cyanosis, or a bluish discoloration of the lips and nail bed
- Lack of energy
- Unintentional weight loss.
Causes of chronic obstructive pulmonary disease?
There are many factors that contribute to the development of COPD. The main cause is cigarette smoking. Other factors are:
- Secondhand cigarette smoke
- Air pollution
- Exposure to chemical fumes and harmful dusts or at work.
In rare cases, non-smokers or children can develop COPD as a result of alpha-1 antitrypsin deficiency (A1AD). A1AD is a genetic disorder caused by abnormally low levels of a protein called alpha-1 antitrypsin. These patients develop emphysema at the base of the lungs.
How is COPD diagnosed and evaluated?
Your primary care doctor will begin by reviewing your medical history and asking about your symptoms. You will also undergo a physical exam.
If your doctor suspects that you have COPD, the following tests may be done:
• Spirometry: This lung function test uses a machine called a spirometer that measures how much air you are able to move when you take a deep breath and exhale, and how quickly you can do so.
• Arterial blood gas analysis: This test measures the amount of oxygen and carbon dioxide in your blood. A high percentage of carbon dioxide in the blood can be a sign of poor lung function caused by COPD.
Your doctor may also order the following imaging tests:
• Chest X-ray – This test can help confirm the diagnosis of COPD by producing images of the lungs that allow symptoms of shortness of breath or chronic cough to be evaluated. Although a chest x-ray may not reveal COPD until it is severe, the images may show enlarged lungs, air pockets (vesicles), or a flattened diaphragm. A chest X-ray may also be used to determine if another condition might be causing COPD-like symptoms. See the Safety Page for more information on X-rays.
• Computed tomography (CT) scan of the chest: This test may be done to help confirm the diagnosis of COPD or to determine if the disease has worsened. It combines special x-ray equipment with sophisticated computers to produce multiple images, or pictures, of the inside of the lungs. CT images can identify emphysema better, and at an earlier stage, than chest X-rays. They can also identify other COPD changes, such as enlarged arteries in the lungs. CT is sometimes used to measure the extent of emphysema in the lungs. It can also help determine if the symptoms are the result of another breast disease.
How is COPD treated?
Although there is no cure for COPD, your doctor may recommend one or more of the following options to help relieve symptoms:
• Lifestyle changes: stop smoking for good and increase physical activity.
• Therapies: Oxygen therapy involves the use of a device that delivers more oxygen to the lungs. Pulmonary rehabilitation is a program that uses counseling, advice about diet, and physical activity to help you better manage your COPD.
• Medications – In an attempt to treat the symptoms of COPD, steroids, inhalers, and antibiotics may be prescribed.
• Surgery: In severe cases, when symptoms have not improved with medications or noninvasive therapies, major surgery, such as a lung transplant or lung volume reduction surgery, may be necessary.
COPD medicine
The information provided here is intended to provide a general idea about each of the medications listed below. Only the most general side effects are included. For this reason, ask your doctor if you need to take any special precautions. Use each of these COPD medicine as directed by your doctor. Be sure to follow the instructions listed. If you have additional questions about use or side effects, ask your doctor.
Various medications can be prescribed to treat COPD. These medications can be taken by mouth or inhaled into the lungs. Some of them work by opening the airways. Others are designed to reduce inflammation or eliminate infection. The following list contains some of these medications. Doctors often choose drugs related to those on the list. They can also choose drug combinations.
Prescription drugs
- Bronchodilators
- Corticosteroids
- Oxygen therapy
- Antibiotics.
Bronchodilators
Short-acting bronchodilators include the following:
- Albuterol (Proventil)
- Terbutaline (Brethine)
- Theophylline (Theobid).
Long-acting bronchodilators include the following:
- Salmeterol (Serevent)
- Formoterol (Foradil)
- Arformoterol (Brovana)
- Ipratropium bromide (Atrovent)
- Tiotropium (Spiriva)
- Theophylline (Theobid).
These COPD medicines work by relaxing the smooth muscles of the respiratory tract, which allows the bronchial tubes to open up and make it easier to breathe. Depending on the medication prescribed, these drugs may be taken orally, inhaled, injected, or given intravenously.
Possible side effects include:
- Accelerated heart rate
- Nervousness, tremors
- Headache
- Heartburn or nausea
- Insomnia
- Constipation with tiotropium
- Dry mouth with tiotropium
- Sore throat with tiotropium.
Corticosteroids
Some common names include:
- Beclomethasone (Beclovent)
- Triamcinolone (Azmacort)
- Budesonide (Pulmicort)
- Flunisolide (AeroBid)
- Fluticasone (Flovent).
Corticosteroids reduce inflammation in the walls of the airways. They are often used if airway obstruction cannot be controlled with bronchodilators. Corticosteroids are usually inhaled, which allows them to act directly on inflamed lung tissue. Few side effects are associated with their use if inhaled.
Possible side effects of inhalation therapy include:
- Headache
- Dry throat or mouth
- Hoarseness
- Fungus in the mouth or throat (oral candidiasis).
Systemic corticosteroids, given orally or intravenously, can also be used to treat exacerbations of COPD. However, long-term use is not usually recommended in those with COPD.
Oxygen therapy
Supplemental oxygen can be given in the hospital or as home oxygen therapy. There are three common ways that oxygen is given. A nasal cannula is a two-pronged device that is inserted into the nostrils and connected to a tube that carries oxygen. The tube can rest on the ears or be attached to the frame of the glasses. People who need a high flow of oxygen usually use a mask.
Some people who use a nasal cannula during the day prefer a mask at night. Masks are also helpful when the nose is sore or stuffy from a cold. Transtracheal oxygen therapy requires a small, flexible tube to be inserted into the trachea. The transtracheal catheter is held in place with a collar.
Oxygen therapy increases low blood oxygen levels. This increases the ability to tolerate exercise and improves mental function. It also improves heart function and helps prevent some of the heart complications of COPD. You may only need oxygen during waking hours, or you may need it all the time throughout the day. Make sure you understand how many hours a day you need to use oxygen. It is important to follow the indication strictly.
If you use supplemental oxygen, it is vitally important that you do not smoke cigarettes. You should also avoid any other sources of fire or flame, such as candles or gas stoves, as they can cause an explosive reaction. You should also avoid drinking alcohol or taking sedatives, as these can slow your rate of breathing.
While receiving supplemental oxygen therapy, contact your doctor if:
- You develop a headache, bluish lips, confusion, or agitation
- Your breathing becomes very shallow
- You are still very tired after light exertion.
Antibiotics
- Tetracycline or doxycycline (Achromycin, Sumycin)
- Ampicillin or amoxicillin (Polycillin, Amoxil)
- Trimethoprim and sulfamethoxazole (Bactrim, Septra)
- Clarithromycin (Biaxin)
- Azithromycin (Zithromax)
- Erythromycin (Emycin, EES)
- Cephalosporins
- Quinolones (ciprofloxacin, levofloxacin).
Antibiotics are used to treat bacterial infections that could further limit breathing. They are usually prescribed at the first sign of a respiratory infection, such as increased production of yellowish or greenish sputum, or fever. They are usually taken for three to seven days. Some are taken with food or on an empty stomach. It is generally best to avoid alcohol while taking antibiotics.
Some of the more likely side effects include:
- Diarrhea
- Headache
- Stomachache
- Sore mouth or tongue
- Vaginal itching due to yeast or candida growth
- Increased sensitivity to sunlight with tetracycline
- Exanthema.
Special considerations
If you have COPD, talk to your doctor before taking any over-the-counter medication.
If you are taking medication, follow these general guidelines:
• Take the medicine as indicated. Do not change the amount or the schedule.
• Learn about the side effects that could occur. Check them out with your doctor.
• Talk to your doctor before you stop taking the medicine.
• Plan ahead for refills if you need them.
• Do not share medications with anyone.
• Some medicines can be dangerous when mixed together. Talk to your doctor if you take more than one medicine, including over-the-counter products and supplements.
When to contact the doctor
Contact your doctor if you:
• You have serious side effects, such as increased shortness of breath or signs of an allergic reaction (eg, swelling of the face, lips, or eyelids).
• You have prolonged nausea, vomiting, or diarrhea
• You notice whiteheads in your mouth or vaginal itching (possible yeast infection )
• You have severe or prolonged muscle cramps or heart palpitations
