Crohn’s disease also known as ileitis is a chronic inflammation of the gastrointestinal tract that usually progresses in bursts. Typical symptoms are abdominal pain and severe diarrhea.
In this article you will read about the causes, symptoms, treatment of Crohn’s disease and Is Crohn’s disease curable?
However, the symptoms can be positively influenced by medication and a corresponding lifestyle. Read here what exactly Crohn’s disease is, what causes the disease and how it can be treated.
Brief overview
- Description : chronic inflammatory bowel disease (IBD), which can also affect the rest of the digestive tract.
- Causes : still unclear, but the following factors may play a role: genetic predisposition, impaired barrier function of the intestine, changed composition of the intestinal flora (intestinal microbiome), environmental factors (such as smoking).
- Common symptoms : cramp-like abdominal pain, diarrhea, weight loss, fatigue, possibly fever, formation of abscesses and fistulas.
- Examinations : physical examination, ultrasound, colonoscopy, gastroscopy, endoscopy, possibly MRI and CT, blood and stool examinations.
- Treatment : mostly with drugs such as cortisone, mesalazine, immunosuppressants (such as azathioprine), biologics, anti- diarrhea agents ; possibly surgery, psychotherapy.
- Prognosis : very different courses and degrees of severity, incurable.
Description of Crohn’s disease

Crohn’s disease is one next to the ulcerative colitis the inflammatory bowel disease (IBD). The main symptoms are cramping abdominal pain and diarrhea. The symptoms usually come on in bursts. The patients can therefore also be symptom-free for a longer period of time.
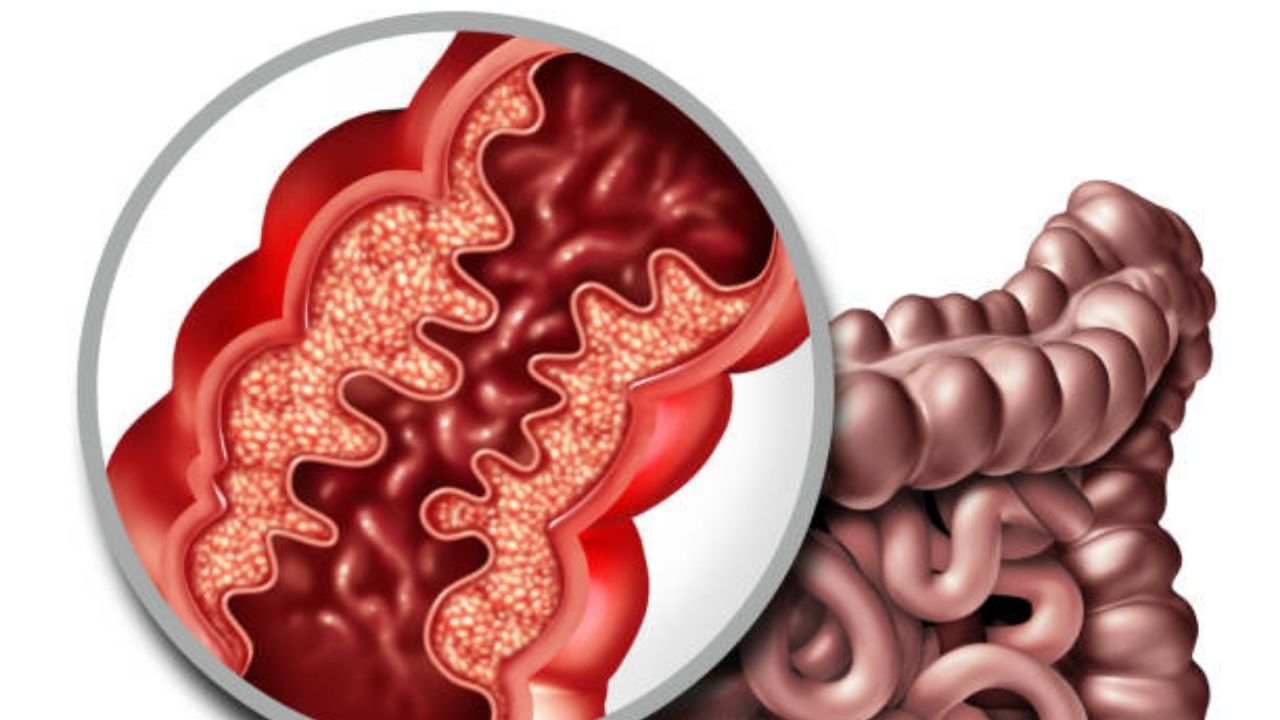
Basically, Crohn’s disease can affect the entire digestive tract – from the mouth to the anus. Usually, however, only the last section of the small intestine and the transition to the large intestine are affected.
Is Crohn’s disease curable?
Crohn’s disease curable or not?
So far, there is no cure for Crohn’s disease so it’s a incurable. Crohn’s disease varies in severity from patient to patient. If the course is unfavorable, ulcers, constrictions (stenoses) and / or connecting ducts (fistulas) to other organs form.
Causes of Crohn’s disease
Crohn’s disease is associated with inflammation of the mucous membrane in the digestive tract – as mentioned above, preferably in the intestine. The inflammatory processes also spread to deeper layers of the intestinal wall.
Adjacent structures such as lymph nodes and the attachment of the intestine (mesentery) can also be affected.
The disease spreads in sections and not continuously in the digestive tract – healthy and diseased sections of the intestine alternate.
Why some people get Crohn’s disease is still not fully understood. Several factors are likely to contribute to the development of the disease:
Genetic factors
Crohn’s disease can be hereditary. Researchers are now familiar with numerous different genes that can be altered in inflammatory bowel disease. One of them is the NOD2 (= CARD15) gene.
It contains the blueprint for a binding site (receptor) which regulates the release of the body’s own antibiotics in the small intestine. People who have one or more changes (mutations) in this gene are at increased risk of developing Crohn’s disease.
Impaired barrier function in the intestine
A possible factor in the development of inflammatory bowel diseases such as Crohn’s disease is a disturbed barrier function of the intestinal wall. On the one hand, the intestine must be permeable so that nutrients can get into the body, but on the other hand, it must also prevent pathogens from entering.
If this balance is disturbed, problems arise. For example, bacteria naturally living in the intestine can penetrate the intestinal mucosa and thus call the immune system on the scene – various inflammatory cells are activated, which could contribute to the development of the disease.
Altered gut microbiome
The microorganisms naturally living in the intestine – collectively referred to as the intestinal microbiome (or intestinal flora) – could also play a role. For example, increased concentrations of a certain bacterium (Myobacterium avium ssp. Paratuberculosis, or MAP for short) were found in the intestines of patients.
This germ triggers what is known as paratuberculosis or Johne’s disease in cattle – a disease with symptoms comparable to those in Crohn’s disease. So some researchers believe that MAP causes Crohn’s disease in humans.
However, the changed microbiome composition could also be a consequence of the intestinal disease and not its cause. In addition, there are also studies in which no increased MAP concentrations were found in the intestines of Crohn’s disease patients.
Environmental factors
Smoking increases the risk of developing Crohn’s disease. Other possible influencing factors on the development of the disease are, for example, eating habits, hygiene and breastfeeding status.
Symptoms of Crohn’s disease
Crohn’s disease is very different. Some patients have very frequent and severe symptoms. Others have milder Crohn’s symptoms. The disease can even go undetected for years.
In most cases, Crohn’s disease progresses in phases – phases with more or less severe symptoms alternate with phases with or without symptoms (phases of remission). However, if a patient has been suffering from symptoms for more than six months, it is called a chronically active course.
Typical Crohn’s disease symptoms are:
- Abdominal pain : The pain in Crohn’s disease is often spasmodic and occurs mainly in the right lower abdomen (this is where the last section of the small intestine is located). So they resemble the symptoms of appendicitis. The pain can also be felt in other abdominal regions or diffusely throughout the entire abdomen.
- Diarrhea : Diarrhea usually occurs several times a day during an attack.
- Weight loss : Because of a lack of appetite and / or fear of abdominal pain, many people do not eat enough. Many nutrients are also lost due to the diarrhea. Because of this, patients often lose a lot of weight.
- Fatigue, exhaustion, possibly fever : Due to the inflammatory processes, the patients feel tired and limp. Some also develop a high temperature or even a fever. This is particularly the case with abscess formation (see below).
- Abscesses and fistulas : The inflammation can cause encapsulated collections of pus (abscesses) to form. Connections (fistulas) to other organs, into the abdominal cavity or to the outside world can also arise. They often occur in the anal area and are often the first indication of Crohn’s disease.
- Deficiency symptoms : Inflamed sections of the small intestine can no longer absorb nutrients as well. The diarrhea also causes nutrients to be lost. In total, deficiency symptoms can develop, for example skin changes (due to zinc deficiency) or aphthous ulcers. Long-term calcium deficiency can also trigger osteoporosis.
Complications of Crohn’s disease
If you also want to know that Is Crohn’s disease curable? So as I told you above, still there is no permanent cure for it. Crohn’s disease is still incurable.
Therefore you are advised that avoiding this disease is a better option.
When the inflamed sections of the intestine heal (temporarily), scars often form. In severe cases, this can lead to an intestinal obstruction (ileus) that requires surgery.
Sometimes Crohn’s disease also affects organs outside the intestine (extraintestinal involvement). Possible consequences and complications are, for example:
- Fatty liver, chronic inflammation of the liver (chronic hepatitis), jaundice, cirrhosis of the liver, abscesses in the liver.
- Gallstones, biliary inflammation, gallbladder cancer.
- Kidney stones.
- Brownish lumps on the lower legs, painful skin ulcers.
- Drumstick fingers, whitish discoloration of the nails.
- Joint inflammation, joint pain, ankylosing spondylitis.
- Iris inflammation.
- Anemia, vascular occlusion due to blood clots (thrombosis).
- Vascular inflammation.
- Inflammation of the pericardium (pericarditis).
- Deposition of protein in various organs (amyloidosis).
- Overactive thyroid gland (hyperthyroidism).
In addition, chronic illnesses such as Crohn’s disease represent a psychological burden for those affected. Many patients withdraw from social life and suffer from depressive moods. Some even develop mental disorders (such as anxiety or obsessive-compulsive behavior).
Treatment for Crohn’s disease
So far there is no cure for Crohn’s disease. However, the treatment can slow down the inflammatory processes of Crohn’s disease. When planning therapy, the doctor takes into account which sections of the digestive tract are inflamed and how severe the disease is.
Most of the time, Crohn’s disease is treated with medication, very often several medications are used together (combination therapy). In severe cases, an operation can be useful.
Medication
Crohn’s disease is all about getting the inflammation under control and relieving the symptoms. For this purpose, drugs are used that have anti-inflammatory effects or change or dampen the activity of the immune system.
If necessary, other medications are also given (e.g. for diarrhea). The following active ingredients or groups of active ingredients can be used in the treatment of Crohn’s disease:
Corticosteroids (“cortisone”)
Cortisone preparations such as prednisolone or prednisone have a strong anti-inflammatory effect. They are usually given as tablets or capsules, sometimes also as an infusion, so that they can develop their effect throughout the body (systemic cortisone therapy). The dosage depends on the severity of the inflammatory activity.
Corticosteroids are given during an acute flare-up, usually for several months. However, experts advise against long-term systemic cortisone therapy. The reason for this are the possible side effects with longer or higher dosed use (eg weight gain, “full moon face”, increased blood sugar and blood lipid levels, increased susceptibility to infections, increased risk of osteoporosis).
The cortisone preparation budesonide mainly works in the intestine and is hardly absorbed by the body. Therefore, it has fewer side effects than other cortisone preparations. Budenoside capsules are prescribed when Crohn’s disease affects only the lower part of the small intestine and the appendix, but no other places in the intestine or the rest of the body.
Mesalazine
Mesalazine (5-aminoslicylic acid, 5-ASA) is also anti-inflammatory, but less effective than cortisone supplements. But it is better tolerated. Mesalazine is used for mild disease processes – sometimes over a longer period of time to prevent the inflammation from flaring up again.
Immunosuppressants
Immunosuppressants downregulate the activity of the immune system and are used for the long-term treatment of Crohn’s disease. Sometimes they are also used in combination with cortisone preparations, for example in the case of chronically active disease.
Frequently used immunosuppressants in Crohn’s disease therapy are azathioprine and mercaptopurine. Another representative is methotrexate – an active ingredient that is also used in cancer therapy (as a cytostatic = agent that inhibits cell growth).
Corticosteroids also have an immunosuppressive effect, but are primarily used in Crohn’s disease therapy because of their strong anti-inflammatory properties.
Biologics
For some patients, Crohn’s disease treatment also includes something called biologics. These are drugs that living organisms (such as bacteria) produce. They can be given for severe flare-ups when cortisone does not help enough. In addition, biologics are used for long-term treatment – instead of or together with immunosuppressants.
Some examples of biologics used in Crohn’s disease:
TNF-alpha antibodies (e.g. infliximab, adalimumab) are so-called monoclonal antibodies and have an anti-inflammatory effect: They specifically block a certain component of the immune system – the inflammatory messenger tumor necrosis factor (TNF). That is why they are also called TNF-alpha blockers.
The drugs are given as an infusion or syringe under the skin. TNF-alpha antibodies are used, for example, when high inflammatory activity cannot be brought under control with cortisone. They are also often prescribed to patients with persistent fistulas.
Monoclonal antibody
It blocks the inflammatory messengers interleukin 12 and 23, which also results in an anti-inflammatory effect. The drug can be prescribed when TNF-alpha blockers do not work well enough.
Vedolizumab – another monoclonal antibody with anti-inflammatory effects – binds to a specific protein on the surface of certain immune cells (lymphocytes). As a result, these can no longer migrate from the blood into the intestinal tissue and trigger inflammation there. Vedolizumab is given as an infusion. It can also be given when other medications do not work well enough against the bowel inflammation.
Other drugs
Depending on your needs, the doctor will prescribe other medications for Crohn’s disease, for example diarrhea medication (e.g. loperamide) to prevent accelerated bowel evacuation or anticonvulsants (e.g. butylscopalamin) to relieve stomach pain. If accumulations of pus (abscesses) or fistulas have formed, the patient is usually given antibiotics (e.g. metronidazole).
Nutrient preparations or nutrient solutions (formula diets) may be necessary if sufficient nutrient absorption is prevented by strong inflammatory processes or constrictions in the intestine.
Operations of Crohn’s disease
Surgery is usually necessary for Crohn’s disease if complications arise such as:
- Rupture of the intestine.
- Bowel obstruction or permanent narrowing of the bowel (bowel stenosis).
- Severe bleeding from the bowel.
- Inflammation of the peritoneum (peritonitis).
Abscesses or fistulas between the intestine and the urinary bladder also often require surgery.
In severe cases of Crohn’s disease, severely inflamed sections of the intestine can be surgically removed. However, this does not cure the disease – the inflammation can later recur in other areas.
Around 70 percent of all Crohn’s disease patients must have an operation within 15 years of being diagnosed.
Diet for Crohn’s disease
There is no evidence that specific diets help with Crohn’s disease. However, a light whole diet (previously known as a basic gastroenterological diet) is recommended in symptom-free or poor phases.
It cannot cure gastrointestinal diseases such as Crohn’s disease, but it can relieve the digestive tract and metabolism. This can prevent unspecific intolerances such as pressure, bloating or flatulence.
The light whole diet is not only recommended for chronic inflammatory bowel diseases (in remission phases = phases between attacks), but also, for example, for irritable bowel syndrome, unspecific food intolerance, gastric and duodenal ulcers and uncomplicated liver and gallbladder diseases.
Concept of light whole food
The light whole food is a wholesome, balanced diet that provides the body with all the nutrients it needs in sufficient quantities. However, if there is a proven nutritional deficiency (e.g. iron deficiency), the attending physician can also prescribe a suitable nutrient preparation.
As with the “normal” wholesome diet, the recommended nutrient composition for light whole foods is :
- 50 to 55 percent carbohydrates.
- 30 percent fat.
- 10 to 15 percent protein.
In contrast to the “normal” whole diet, the light whole diet dispenses with food and drinks, which, as experience has shown, are often poorly tolerated in the case of gastrointestinal diseases. These include, for example:
- Whole milk and full-fat dairy products, cream and sour cream with over 20% fat, spicy and fatty cheeses (45% fat), blue cheese.
- Fatty, smoked, cured and seared meat, fatty and smoked sausage products.
- Fat soups and sauces.
- Fatty fish (such as eel, herring, salmon), smoked fish, pickled and / or preserved fish and fish products.
- Hard-boiled eggs, mayonnaise.
- Large amounts of oil, butter, normal margarine, lard and tallow.
- Fresh bread, coarse wholemeal breads, fresh or fatty baked goods (such as cream cake, puff pastry, fried foods).
- Fried and fried potato dishes (French fries, fried potatoes, etc.), potato salad with bacon, mayonnaise or lots of oil.
- Generally dishes that have been seared, roasted, deep-fried or seared with bacon and onions.
- Vegetables that are difficult to digest and bloat (e.g. cabbage, onions, leeks, peppers, cucumbers, legumes, mushrooms), salads prepared with mayonnaise or fatty sauces.
- Unripe fruit, raw stone fruit, nuts, almonds, pistachios, olives, avocados.
- Chocolate, pralines, nougat, marzipan, cream candies etc.
- Large amounts of sugar.
- Large amounts of salt, pepper, curry, paprika powder, mustard, horseradish, onion or garlic powder, hot spice mixtures.
- Alcohol, carbonated drinks (such as soda, cola), ice-cold drinks.
- Bear in mind that everyone’s sensitivity to certain foods and drinks is different. For example, some Crohn’s disease patients can easily consume small amounts of whole milk or a candy bar, while others respond with discomfort. Try out which products you can tolerate and in which quantities!
- When it comes to grains and grain products, whole grains should be preferred and white flour should be avoided. Whole grains provide the body with a lot of fiber, which aids digestion.
Caution: If Crohn’s disease patients have extensive constrictions (stenoses) in the intestine, the diet should be low in fiber!
General nutrition tips
- Give yourself plenty of time while eating and chew each bite thoroughly.
- Don’t eat too hot or too cold, not too sour or too spicy.
Diet during a attack
The stomach and intestines need special protection during an attack. Most patients can then tolerate a light, low-fiber diet. Puree the food can also have a relieving effect. In the event of a severe episode, temporary artificial nutrition via drip may also make sense so that the digestive tract can calm down.
psychotherapy
Persistent toilets, abdominal pain, fatigue – in severe cases, Crohn’s disease has a massive impact on the patient’s quality of life and self-esteem. Some people even develop mental disorders such as depression or anxiety disorders.
Psychotherapy can help to cope better with the stress and to develop a positive attitude towards life and a stable self-image despite the illness.
As part of cognitive behavioral therapy, the patient questions and corrects negative thought patterns and practices new behaviors. Since stress can also worsen the symptoms, patients learn strategies that will help them avoid unnecessary emotional stress.
Stress reduction
Individual with Crohn’s disease benefit from learning a relaxation methods. In this way, stress can be relieved, which can adversely affect the course of the disease. Examples of helpful methods are:
- Autogenic training.
- Progressive muscle relaxation.
- Meditation.
Diagnosis of Crohn’s disease
In order to be able to make the diagnosis of Crohn’s disease, there are several steps. The beginning is a detailed doctor-patient discussion to collect the medical history. The doctor asks, among other things, which symptoms the patient has and when they first appeared. He also asks whether there are cases of inflammatory bowel disease (Crohn’s disease, ulcerative colitis) in the family. Various investigations followed the conversation.
Physical examination
As part of a physical examination, the doctor palpates the patient’s stomach and checks whether there is any pressure pain.
Ultrasound
An ultrasound device can be used to detect inflammatory thickened intestinal walls, constrictions, fistulas and abscesses. Changes in the mucous membrane can only be found with an endoscopic examination.
A doctor can also use ultrasound to regularly check the course of Crohn’s disease.
Colonoscopy
A colonoscopy is the most important test used to diagnose Crohn’s disease. The doctor carefully inserts a flexible endoscope – a thin tube with a tiny camera and a light source at the tip – through the anus into the intestine. This allows him to take a closer look at the intestinal mucosa.
The doctor can also use the endoscope to insert fine instruments into the intestine, for example to take a tissue sample (biopsy). This is examined more closely in the laboratory for pathological changes. Constrictions (stenoses) and fistulas can also be detected in the colonoscopy and, if necessary, treated immediately.
Gastroscopy
In gastroscopy, an endoscope is inserted through the mouth into the stomach – up to the transition to the first section of the small intestine (duodenum). In this way, the doctor can check whether there are any foci of inflammation in the upper digestive tract.
Capsule endoscopy
In unclear cases, the doctor also performs other endoscopic examinations – such as capsule endoscopy. The endoscope is a small capsule the size of a tablet and is swallowed by the patient.
The integrated small camera with a light source records images of the inside of the intestine on its way through the digestive tract and sends them wirelessly to sensors that are attached to the outside of the patient’s body. A recorder that is worn on the belt stores the data. The capsule is eventually excreted naturally (in the stool).
MRI and CT
Also by means of MRI (magnetic resonance imaging), the intestine can be examined more closely pathological changes. In addition, it can be used to detect fistulas and abscesses and display them in detail, just as with computed tomography (CT).
Blood and stool tests
If there is severe inflammation anywhere in the body, this is reflected in certain blood values: C-reactive protein (CRP), white blood cells (leukocytes) and blood sedimentation (ESR) are usually increased. So these parameters act as non-specific signs of inflammation.
Blood tests can also point to nutrient deficiencies that have developed as a result of chronic bowel inflammation – such as a deficiency in zinc, calcium, vitamin B12, folic acid or iron.
Other blood values (such as kidney or thyroid values) may be changed if Crohn’s disease has affected organs other than the intestines
Stool exams are used to rule out other causes of common diarrhea with abdominal pain (such as bacterial infections).
Crohn’s disease course and prognosis
There is no complete cure for Crohn’s disease. The course of the disease varies greatly from patient to patient and cannot be predicted. While some patients are completely symptom-free for a long time or have only few pronounced symptoms, others experience frequently recurring, severe phases of the disease or have a chronic course of the disease.
As a person affected, you can do a lot yourself to reduce the severity of your symptoms and to extend the symptom-free phases:
- Consistently take the prescribed medication.
- Get enough sleep.
- Relax regularly.
- Eat what is good for you. But make sure you eat a balanced diet – malnutrition can aggravate the clinical picture or even encourage relapses (relapses)!
- Contact your doctor immediately if you feel that a new flare-up of illness is imminent (e.g. with increased abdominal pain). He can readjust your medication if necessary and thus counteract the flare-up or identify and treat possible complications at an early stage.
Also, get regular colon cancer screenings – people with Crohn’s disease are at a slightly higher risk of developing a malignant colon cancer.
With proper treatment, the life expectancy of people with Crohn’s disease is normal.