Wegener’s granulomatosis also called granulomatosis with polyangiitis is a chronic, inflammatory disease of the blood vessels with small, knot-like thickening of the skin (granulomas). If left untreated, it spreads throughout the body and can be fatal. The symptoms can be alleviated, but the rare disease cannot be cured.
Read everything you need to know about granulomatosis with polyangiitis here. Such as symptoms, causes, diagnosis and treatment of wegener’s granulomatosis.
ICD codes for this disease: M31
Definition of wegener’s granulomatosis
Wegener’s granulomatosis is a rare inflammation of the blood vessels (vasculitis) accompanied by the formation of small tissue nodules in the affected areas. This leads to circulatory disorders and a reduced supply of oxygen and nutrients to the tissue in the affected organs.
The term “granulomatosis” refers to the formed tissue nodules (= granulomas). “Polyangiitis” means inflammation of many vessels.
Granulomatosis with polyangiitis is a systemic disease. This means that, in principle, several organ systems can be affected. As a rule, wegener’s disease initially affects the upper respiratory tract and, in later stages, also internal organs. In addition, granulomatosis with angiitis can affect the ears and eyes.
It becomes dangerous as soon as the lungs or kidneys are affected. In extreme cases, acute pulmonary hemorrhage or acute kidney failure can occur. Both complications can be fatal.
History of name
Until 2011, granulomatosis with polyangiitis was known as Morbus Wegener (also known as Wegener’s granulomatosis or Wegener’s granulomatosis). The name change recommended by American and European rheumatism associations is based on the controversial role of the former namesake Friedrich Wegener during the National Socialist era.
Symptoms of wegener’s granulomatosis
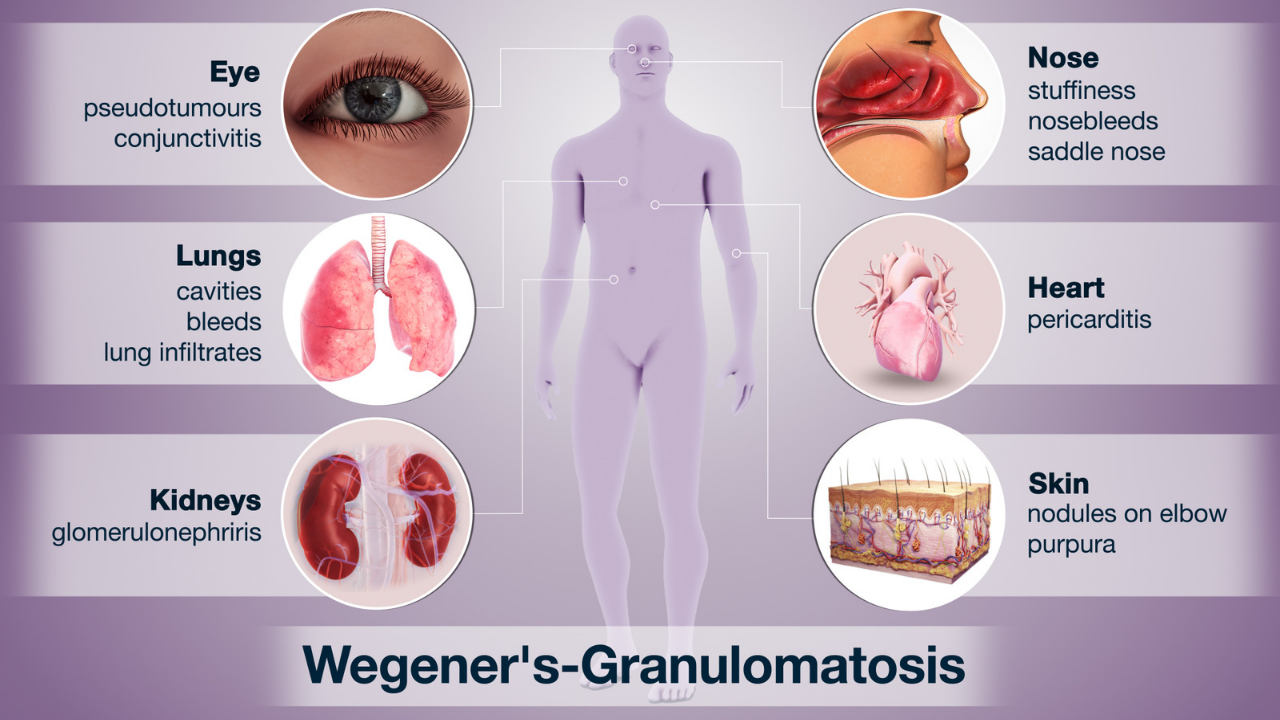
wegener’s granulomatosis symptoms – Granulomatosis with polyangiitis can affect different organ systems. Which organs are affected and to what extent varies from patient to patient.
In addition, the symptoms of Wegener’s disease develop as the disease progresses: In the early stages, the symptoms are mainly in the ear, nose and throat area. If left untreated, granulomatosis later spreads to other organs, some of which are vital.
Symptoms in the early stages
At the beginning of the disease, the nasal mucous membranes are usually affected. Associated symptoms include in particular:
- (Bloody) cold with a constantly runny or chronically blocked nose.
- Nosebleeds.
- Brownish crusts on the nose.
- Saddle nose : The constant inflammatory processes can change the nasal septum in such a way that a saddle-shaped sunken nose develops.
Starting from the nose, granulomatosis with polyangiitis (Wegener’s disease) can spread further into the paranasal sinuses and cause inflammation there (inflammation of the paranasal sinuses, sinusitis). Pain in the jaw or forehead area that is difficult to localize can indicate this.
If the disease spreads further, a middle ear infection (otitis) can develop. This manifests itself primarily in the form of severe earache, sometimes associated with dizziness. In extreme cases, granulomatosis with polyangiitis can even lead to deafness.
General symptoms such as fever, night sweats, weight loss, a general feeling of illness and weakness and increased tiredness also appear in the early stages of the disease.
Symptoms later
As the disease progresses, the symptoms of inflammation spread further and further throughout the body. The following are particularly affected:
- Throat: Hoarseness, dysphagia or a dry cough appear when the granulomatosis with polyangiitis spreads in the throat and pharynx.
- Muscles and joints: Painful swelling and tenderness occur in the joints, especially in the legs and arms. Muscle pain can also occur.
- Lungs, pleura, heart : In about 60 percent of Morbus Wegener patients, the disease affects the lungs after some time. A frequent result is pneumonia with a bloody cough. The inflammation can spread from the lungs to the pleura (pleurisy). Inflammation of the pericardium (pericarditis) with subsequent cardiac effusion (cardiac tamponade) is also possible.
- Eyes: Around 50 percent of those affected suffer from eye pain, burning eyes, eye inflammation or visual disturbances (loss of vision) during the course of granulomatosis with polyangiitis (Wegener’s disease). Bleeding in the eye as well as red patches of skin and small skin nodules around the eye are sometimes visible from the outside.
- Kidneys: The kidney vessels also become inflamed in around 50 percent of those affected by granulomatosis (glomerulonephritis). The classic sign of this is visible traces of blood in the urine (macrohematuria). High blood pressure (hypertension) and the so-called nephrotic syndrome with water retention in the tissue (edema) also occur.
- Skin : Blisters and spot or area discolouration may appear on the skin. These are caused by the death (necrosis) of tissue. If larger blood vessels under the skin are also involved, your doctors speak of gangrene. Such skin symptoms occur in around 20 percent of granulomatosis cases.
- Nervous system: In about 10 percent of cases, granulomatosis extends to the central or peripheral nervous system. Possible consequences are numbness and abnormal sensations in fingers and toes (polyneuropathy). Unsteady gait, headaches and weakness of the extremity muscles occur less frequently. Meningitis can also develop.
Causes of wegener’s granulomatosis
The exact cause of granulomatosis with polyangiitis is not yet known. Scientists suspect that the disease is due to a malfunction of the immune system (autoimmune disease): Due to a malfunction, the immune system forms antibodies against the body’s own cells, in this case blood cells.
An infection of the nasal mucosa with bacteria such as Staphylococcus aureus is discussed as a triggering factor for this malfunction. Parts of the bacteria can activate certain immune cells, which then trigger an excessive immune response against the body’s own cells.
Who does this disease affect?
Wegener’s granulomatosis can affect people of all ages. Most of the affected groups are those between 40 and 60 years of age. It affects men and women alike.
Diagnosis of wegener’s granulomatosis
If there is a suspicion of Morbus Wegener, this should be clarified as quickly and carefully as possible. This enables rapid treatment if granulomatosis with polyangiitis is actually present.
The first point of contact if you suspect granulomatosis is your general practitioner or a specialist.
wegener’s granulomatosis diagnosis:
Medical history
First, the doctor will take your medical history (anamnesis). Here you have the opportunity to describe your symptoms in detail. Even small things that you may find unimportant or irrelevant can help the doctor to find out the cause of the symptoms. In addition, the doctor can ask questions such as
- When did you first notice the changes (e.g. tissue nodules)?
- Have you noticed any other symptoms?
- Have you noticed blood in your urine?
- Do you have pain when you cough or when you breathe heavily, for example when you exercise?
Blood test
As a rule, a blood count is taken first to clarify the suspected diagnosis.
The detection of c-ANCA is regarded as an almost certain indication of Wegener’s granulomatosis. The abbreviation stands for cytoplasmic anti-neutrophil cytoplasmic antibodies. These are certain autoantibodies against certain blood cells. c-ANCA can be detected in the vast majority of all patients with Wegener’s disease.
However, these autoantibodies are also found in some other diseases (such as tuberculosis) in the blood of those affected. Therefore, an elevated c-ANCA value alone is not sufficient to diagnose granulomatosis with polyangiitis.
An increased blood cell sedimentation rate (ESR, blood sedimentation) is also considered an indication of Wegener’s granulomatosis if it is accompanied by an increased number of white blood cells (leucocytosis). On their own, however, none of these values is evidence of Wegener’s disease.
Urine test
The doctor can use a urine test to find out whether the kidneys are affected. In the case of kidney weakness (renal insufficiency), an increased creatinine value can be measured in the urine.
Glomerulonephritis is blood in the urine (hematuria): In the early stages of the disease, there are tiny traces of blood that can only be seen under a microscope (microhematuria). In later stages, the blood can also be seen with the naked eye.
Tissue samples
Tissue samples (biopsies) from the nasal mucosa, for example, are very revealing. If the doctor suspects that internal organs (such as lungs, kidneys) are already affected, tissue samples can also be taken from them. If corresponding inflammatory changes are found in the samples, this secures the diagnosis of granulomatosis with polyangiitis (Wegener’s disease).
Treatment of wegener’s granulomatosis
granulomatosis with polyangiitis treatment – Active Wegener’s granulomatosis causes inflammation of blood vessels and organs. Ongoing inflammation of the blood vessels or organs can lead to organ failure. If left untreated, wegener’s granulomatosis can rapidly worsen and lead to life-threatening kidney or lung failure.
Treatment options for wegener’s granulomatosis are based on the organs affected, the severity of the disease, and the individual’s medical complications.
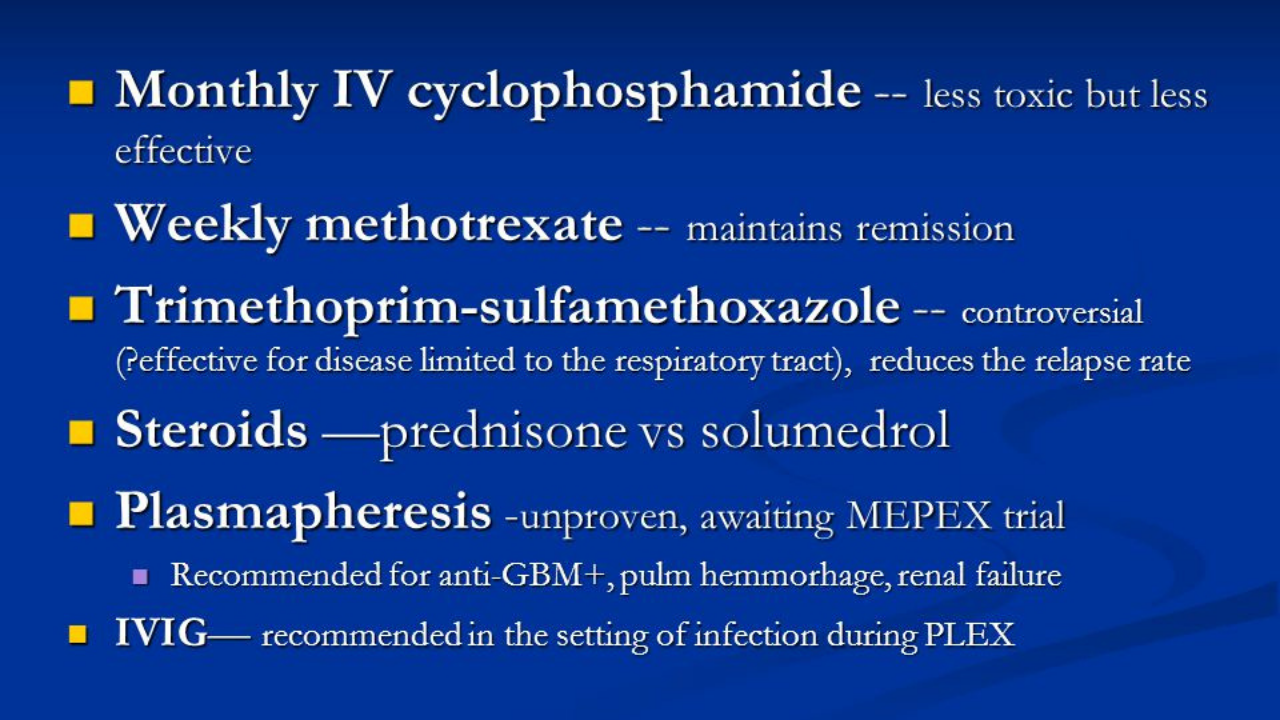
In cases where the disease is active and severe, glucocorticoid (steroid) medications such as prednisone combined with cyclophosphamide (Cytoxan), a type of chemotherapy, are often given. High-dose prednisone is started and then gradually reduced over weeks or months.
Cyclophosphamide is given for 3 to 6 months, either by mouth or by injection. Those who get better are switched to another medication, such as methotrexate (Rheumatrex, Trexall) or azathioprine (Imuran, Azasan) for two years or more.
Another treatment option for severe cases of granulomatosis with polyangiitis is rituximab (Rituxan) combined with glucocorticoids. Rituximab is a medication given as an intravenous injection, which stops the inflammation of the blood vessels and organs.
The patient and his doctor will decide together which is the most appropriate treatment to follow. Patients with less active disease can be treated with prednisone and methotrexate. Both medications have possible side effects that must be considered as part of the treatment plan.
As with many other diseases, the earlier granulomatosis with polyangiitis is detected, the higher the chance of successful treatment of wegener’s granulomatosis.
Acute therapy
The stage of the disease has a significant influence on how the therapy in acute cases looks like in the case of Wegener’s disease – the decisive factor is whether vital organs are affected and/or there is an acute danger to life or not:
No danger to life or involvement of vital organs
In such cases, treatment of wegener’s granulomatosis consists of the combined administration of drugs that suppress the immune system (immunosuppressive combination therapy): The patients receive prednisolone (a cortisone) and either methotrexate (MTX) or mycophenolate mofetil.
Danger to life or involvement of vital organs
If organs such as the lungs or kidneys are already affected by the disease, aggressive immunosuppressive combination therapy is indicated. High-dose prednisolone is combined with either cyclophosphamide or rituximab.
In severe cases, plasmapheresis can also be performed if necessary:
In this complex procedure, blood is drawn out of the patient’s body via an infusion tube and into the plasmapheric device. This device uses a centrifuge to separate the liquid component of the blood (blood plasma or plasma for short) from the solid components (red blood cells, etc.) and replaces it with a replacement liquid – a mixture of electrolytes and hydrogen carbonate. The blood is then returned to the patient’s body.
The purpose of it all: During plasmapheresis, the antibodies in the plasma that are involved in the inflammatory processes in granulomatosis with polyangiitis (Wegener’s disease) are also removed.
Maintenance therapy (maintenance in remission)
If an improvement in symptoms (remission) was achieved with the acute treatment, maintenance therapy for at least 24 months follows. The aim is to permanently maintain the freedom from symptoms achieved through the acute treatment.
The immunosuppressant azathioprine (alternatively rituximab, MTX or mycophenolate mofetil) and the glucocorticoid prednisolone are preferably used. Co-trimoxazole can also be given.
Repeated treatment
It is important to note that all treatment measures can only alleviate the symptoms. Wegener’s granulomatosis is not curable. In more than half of all patients, the symptoms return within two years after successful therapy.
These can then be treated in the same way as with the first therapy. As the disease progresses, relapses with severe symptoms can occur again and again.
What are some of the side effects of treatment?
Because the treatment medications suppress the immune system, there is an increased risk of developing serious infections. Each of the immunosuppressive drugs has a unique collection of potential side effects. Watching for side effects associated with each medication is critical to preventing and minimizing their occurrence.
In addition, the fact that a patient tolerates treatment of wegener’s granulomatosis initially does not guarantee that tolerance will remain the same over time. This makes ongoing monitoring essential, and in some cases, monitoring for long-term side effects may be important, even after the medication has been stopped.
Prognosis of granulomatosis with polyangiitis
Timely treatment of wegener’s granulomatosis can counteract the spread of inflammation in granulomatosis with polyangiitis. In 75 percent of those affected, the symptoms then completely resolve.
However, the disease often breaks out again over time, which then requires immunosuppressive combination therapy each time. With optimal treatment, however, 85 percent of all patients with Morbus Wegener are still alive after five years.
In contrast, the prognosis without treatment is very poor. The further the inflammation spreads in the body, the greater the potential damage. These include, for example, deafness or pulmonary fibrosis.
If the kidneys are affected, death from kidney failure usually occurs within six months. In general, if Wegener’s disease is untreated, the mean survival time is less than one year.
Is it hereditary?
Wegener’s granulomatosis is not hereditary.
It is contagious?
Wegener’s granulomatosis is not a contagious disease.
How rare is wegener’s granulomatosis?
Wegener’s granulomatosis is a rare inflammation of the blood vessels. The prevalence of granulomatosis with polyangiitis in the United States is estimated to be three cases per one hundred thousand people.
Living with granulomatosis with polyangiitis (GPA)
The effect of wegener’s granulomatosis can vary widely, depending on severity, organs affected, and complications related to the disease or treatment of wegener’s granulomatosis.
People with GPA need regular checkups, including lab tests, diagnostic imaging, and seeing their doctor. Follow-up control is essential for patients suffering from wegener’s granulomatosis.
It is important that the doctor look for possible symptoms of the disease returning, and try to detect and avoid short-term or long-term complications of treatment of wegener’s granulomatosis.
Even when treatment is effective, recurrences are common. Recurrences can be similar or different from the initial manifestation, so new symptoms should be reported to the doctor as soon as possible.
Regular medical visits and monitoring of lab tests and diagnostic imaging can help detect recurrences early.
Key points
- In granulomatosis with polyangiitis, the vasculitis involves small and medium-sized vessels in any organ, usually the kidneys (with glomerulonephritis), and the upper and lower airways with significant necrotizing granulomatous inflammation of the parenchyma, which is often more conspicuous than vasculitis.
- Manifestations can affect multiple organ systems and often include upper and lower airway symptoms (eg, recurrent nasal discharge or epistaxis, cough), followed by hypertension and edema (due to renal involvement).
- Confirm the diagnosis with ANCA (antineutrophil cytoplasmic autoantibodies) tests and biopsy.
- Relapses are common, and treatments may contribute to morbidity.
- Remission is induced with corticosteroids plus an immunosuppressant.
- Maintain remission with methotrexate, azathioprine, or rituximab and tapering corticosteroids.
