Hay fever (pollen allergy, seasonal allergic rhinitis) is what doctors call hypersensitivity of the immune system to the proteins of various plant pollens. Around ten to 20 percent of people in Europe are affected. A stuffy, runny and itchy nose and red, itchy eyes are the main symptoms of hay fever. You can read more about the symptoms, causes and treatment of hay fever here.
ICD codes for this disease: J30
Hay fever: Description
According to studies, about ten to 20 percent of people in Europe suffer from hay fever. This is the most common form of allergy. As with all allergies, the body’s immune system overreacts to actually harmless substances in hay fever – but not to hay, as the name suggests, but to proteins from plant pollen in the air.
That is why hay fever is also known as pollen allergy, pollinosis or seasonal allergic rhinitis. “Seasonal” because the various pollens that can cause hay fever are not present in the air all year round, but only during the flowering period of the respective plants. This means that hay fever symptoms only occur in certain months of the year.
If you have hay fever-like symptoms all year round, you probably do not have hay fever, but another form of allergy (e.g. against house dust mites).
Symptoms of hay fever
People without hay fever can often hardly imagine how stressful the symptoms of a pollen allergy actually are: the itchy, watery eyes and the violent attacks of sneezing with a runny nose significantly reduce the quality of life of those affected.
In addition, allergic asthma often develops after a few years due to hay fever. Doctors also refer to this process as a change of floor, since the symptoms spread from the upper respiratory tract deeper into the respiratory tract (lungs and bronchi).
Causes and risk factors

As with all allergies, the symptoms of hay fever (pollen allergy) are caused by an excessive reaction of the immune system: the body’s defense system mistakenly classifies the harmless proteins as dangerous and fights them like a pathogen:
Certain immune cells – the so-called mast cells – release inflammatory messengers (histamine, leukotrienes) when they meet the pollen proteins, which then cause the typical hay fever symptoms. These appear in the area of the eyes, nose and throat, because the pollen proteins enter the body primarily here via the mucous membranes.
Often people with hay fever also develop allergies to certain foods. One then speaks of a cross allergy.
How does the dysregulation of the immune system arise?
The processes involved in the development of pollen allergy have now been well researched. There are only guesses as to what ultimately triggers hay fever. Some risk factors are likely to contribute to the development of hay fever:
Inheritance
Some people are more prone to allergic reactions than others. The allergic reaction readiness is genetically determined and is called atopy. It is hereditary. However, this does not mean that every child of parents with allergies will also become allergic themselves, only the risk of this is increased, as the following comparison shows:
- If no family member is allergic, children have an allergy risk of about 5 to 15 percent.
- If a parent or sibling has an allergy, the risk is about 25 to 30 percent.
- If both parents are allergic, there is a 40 to 60 percent chance that the child will also develop an allergy.
- If both parents have the same allergy, the child’s risk of allergy is about 60 to 80 percent.
Those who are prone to allergies often have more than one. Neurodermatitis patients often tend to get hay fever, and many pollen allergy sufferers cannot tolerate animal hair either.
Excessive hygiene
The extent to which the immune system is challenged during childhood may also play a role in the development of an allergy (hay fever, etc.). The so-called hygiene hypothesis assumes that the body’s defenses are not challenged when there is a lot of hygiene in childhood and that this is why at some point it will also take action against harmless substances.
Observations show that children who grow up with siblings or attend a crèche are less likely to suffer from allergies later on. Children who grow up in a rural environment (e.g. on a farm) also have a lower risk of allergies.
Contact with many other people (other children) or with “dirt” could be “training” for the immune system, while excessive hygiene undertaxes the immune system and thus promotes the development of an allergy.
Tobacco smoke and other air pollutants
Substances in the ambient air that irritate the airways (fine dust, cigarette smoke, car exhaust fumes, etc.) can contribute to the development of allergies (hay fever, etc.) and asthma. For example, children who grow up with parents who smoke have a greatly increased risk of developing asthma, hay fever or other allergies later on.
But even smoking during pregnancy is dangerous for the child, since the components of tobacco smoke can lead to numerous malformations and developmental disorders (e.g. in the lungs). An expectant mother should therefore never smoke during pregnancy. Smoking should generally be taboo in the presence of the child later on.
More and more people suffer from hay fever
Around ten to 20 percent of people in Europe are already struggling with hay fever (allergic rhinitis). Experts from allergological societies assume that this number will continue to rise: in 2050, every second person could be sensitized to at least one type of pollen.
Researchers see climate change as an important reason for the increasing frequency of hay fever: Rising temperatures around the world are significantly lengthening the pollen season for many plants. The higher carbon dioxide (CO2) content in the air also encourages the plants to release even more pollen than before.
In addition, the warmer temperatures make it easier for “foreign” plants to spread into Europe. This applies, for example, to ragweed (ragweed) from the USA: It releases highly allergenic pollen around mid-August to mid-September, which is the main trigger for allergies (such as hay fever) in the USA.
Air pollution from fine dust or ozone pollution also causes the pollen proteins to trigger even more violent reactions. Researchers at the Max Planck Institute for Chemistry in Mainz assume that birch pollen, for example, has a chemical reaction with ozone (O 3) that makes it two to three times more aggressive.
Diagnosis of hay fever
The right contact person if you suspect hay fever (allergic rhinitis) is a doctor with the additional qualification “Allergology”. These are mostly dermatologists, ear, nose and throat (ENT) doctors, lung specialists, internists or paediatricians who have completed additional training as allergists.
Initial consultation
During the first visit, the doctor will first collect the medical history in a detailed discussion. He can usually tell from the description of the symptoms whether it is hay fever. Possible questions from the doctor could be, for example:
- What complaints do you have?
- When exactly do the symptoms appear, i.e. at what time of day and year?
- Where do the symptoms occur – outdoors or just indoors?
- Do you already have allergies?
- Do you have neurodermatitis or asthma?
- Do your parents or siblings have allergic diseases such as asthma, hay fever or neurodermatitis?
- Where do you live (in the country, next to a busy road, etc.)?
- Do you take medicine?
The doctor can determine with relative certainty whether it is hay fever simply by talking about the medical history. Finding the triggering allergen, on the other hand, is sometimes very difficult and resembles detective work.
The first step is to look at the pollen count calendar. The times at which the various plants usually release their pollen are listed there: For example, if you already have typical hay fever symptoms in January, you are probably overreacting to the pollen from alder and/or hazel.
Further investigations
Various diagnostic tests are available to identify the type or types of pollen to which someone is allergic. The examinations include a skin test, provocation test and, if necessary, a blood test for antibodies against pollen proteins (IgE antibodies).
Three days before a skin test and provocation test, the patient should stop taking medication that suppresses allergic reactions (such as cortisone or antihistamines). Otherwise the test result will be falsified.
Prick test: The doctor or an assistant pricks the patient’s skin in several places with a fine needle and drips various allergen-containing solutions (e.g. with proteins from birch pollen, hazel pollen, etc.) onto these small wounds. After a certain time, he examines the reaction of the skin and can see which allergens have caused an allergic reaction (such as reddening of the skin).
Provocation test: The doctor applies the suspected substance to the nose, to the bronchial or conjunctival mucosa of the patient. If the reaction is positive, the mucous membranes swell and symptoms arise.
This test can lead to further, sometimes severe allergic reactions (up to and including anaphylactic shock), which is why the patient should then remain under medical supervision for at least half an hour.
Blood test for antibodies: The “RAST” test can be used to examine whether the patient’s blood contains certain antibodies (specific immunoglobulins IgE) against pollen proteins. The more such antibodies against pollen protein circulate in the blood, the stronger the allergic reaction.
Hay fever in children
Babies and toddlers can also get hay fever. The doctor usually refrains from carrying out a skin test and a provocation test, since both are uncomfortable for the children and the offspring usually vehemently resist them.
Hay fever in pregnancy
Even with hay fever during pregnancy, the doctor should refrain from a prick test and a provocation test because of the potential allergic overreaction (anaphylactic reaction).
Treatment of hay fever
The doctor has various options for treating a pollen allergy. Many patients are given medication to relieve hay fever symptoms. These include, for example, antihistamines. They are available as a nasal spray and in tablet form.
Another way of treating hay fever is hyposensitization. The aim is to gradually get the affected person’s immune system used to the pollen proteins.
Hay fever prevention tips
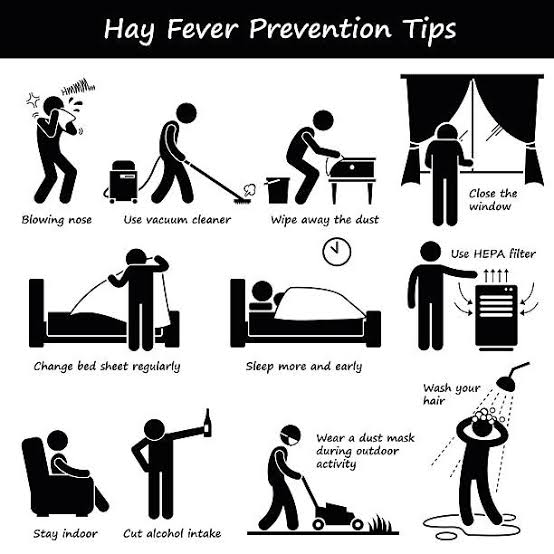
The safest method of not getting hay fever symptoms in the first place is – in addition to specific immunotherapy – avoiding pollen. However, this is not easy, especially since they are floating hundreds of kilometers through the air and can therefore trigger hay fever even if the plants in question are not yet in bloom at the place of residence. However, the following tips can help:
Travelling: If you have the opportunity, you should travel to areas where the plants in question are not yet or no longer blooming when the pollen season of “their” plants. Alternatively, people who are allergic to pollen can also drive in regions where these plants do not occur at all, such as in the high mountains at altitudes of over 2,000 meters, in coastal areas or on islands. There is a general lack of pollen.
Only ventilate at certain times: In rural areas, the pollen concentration is highest between 4 and 6 a.m., which is why people with hay fever should only ventilate in the evening between 7 p.m. and midnight.
It is the other way around in the city: there the pollen concentration is lowest in the morning between six and eight o’clock, which is why the city should be ventilated in the morning hours.
Attaching a pollen screen to the window: A pollen screen looks similar to an insect net. It not only keeps flies and mosquitoes away, but above all prevents pollen from entering the living space. A pollen protection screen on the bedroom window is recommended, especially for hay fever patients who like to sleep with the window open.
Keep the bedroom pollen-free: Taking off your street clothes in front of the bedroom and washing your hair before going to bed prevents pollen from spreading in the bedroom. If possible, freshly washed laundry (e.g. bed linen) should not be dried outdoors, otherwise pollen can adhere to it.
Remove pollen from your living space: hang up a wet towel in your home, the pollen will stick to it. In addition, daily vacuuming and regular dusting are advisable during the pollen season to remove pollen from carpets and furniture.
However, hay fever patients should leave the vacuuming to someone else and should not be present during this time, as this will stir up the pollen. Alternatively, those affected can get a special fine dust mask from the hardware store (so-called FFP3 fine dust mask) for this housework.
Pay attention to the pollen forecast: There are now numerous ways to find out about the current pollen count, similar to the weather. Radio, newspapers and above all the Internet offer regular pollen forecasts for your own region. On days with high pollen levels, hay fever patients should avoid strenuous physical activities as much as possible. Those affected may also need more medication if they have a high pollen load.
Obtain a pollen count calendar: A pollen count calendar offers hay fever patients an approximate orientation as to when they should expect symptoms. This can be very useful for holiday planning, for example. Pollen count calendars are also available free of charge in almost all pharmacies.
Pollen protection when driving: in the car, pollen allergy sufferers should turn off the ventilation and keep the windows closed. With many car models, it is also possible to retrofit the ventilation systems with pollen filters. This is a worthwhile investment if you have severe hay fever, as uncontrollable sneezing attacks while driving have a major impact on road safety.
Rain instead of sun: Rain reduces the concentration of pollen in the air. People with hay fever should therefore prefer to use rain showers and the time shortly afterwards for walks.
Hay fever: course of the disease and prognosis
Many sufferers have hay fever relatively early, i.e. in childhood or adolescence. Ultimately, however, it can occur for the first time in any phase of life.
The pollen allergy usually lasts a lifetime and usually increases in intensity without treatment. Above all, the change of floor, i.e. the spread of the pollen allergy to the respiratory tract to allergic asthma, poses a problem here. With the right therapy, however, the symptoms can be significantly alleviated and possible complications of hay fever prevented.
