Leprosy is an infectious bacterial disease whose symptoms vary depending on the severity of the disease. With timely diagnosis and treatment, the prognosis is favorable and leprosy can be cured with appropriate medication. Read everything you need to know about leprosy here.
ICD codes for leprosy: B92 | A30
Quick overview
- Symptoms: The symptoms depend on the respective form of the leprosy. Symptoms may include skin changes, loss of tactile sensation, and paralysis.
- Prognosis: Leprosy is curable if treated properly. However, if not treated early, the disease can lead to progressive and permanent damage.
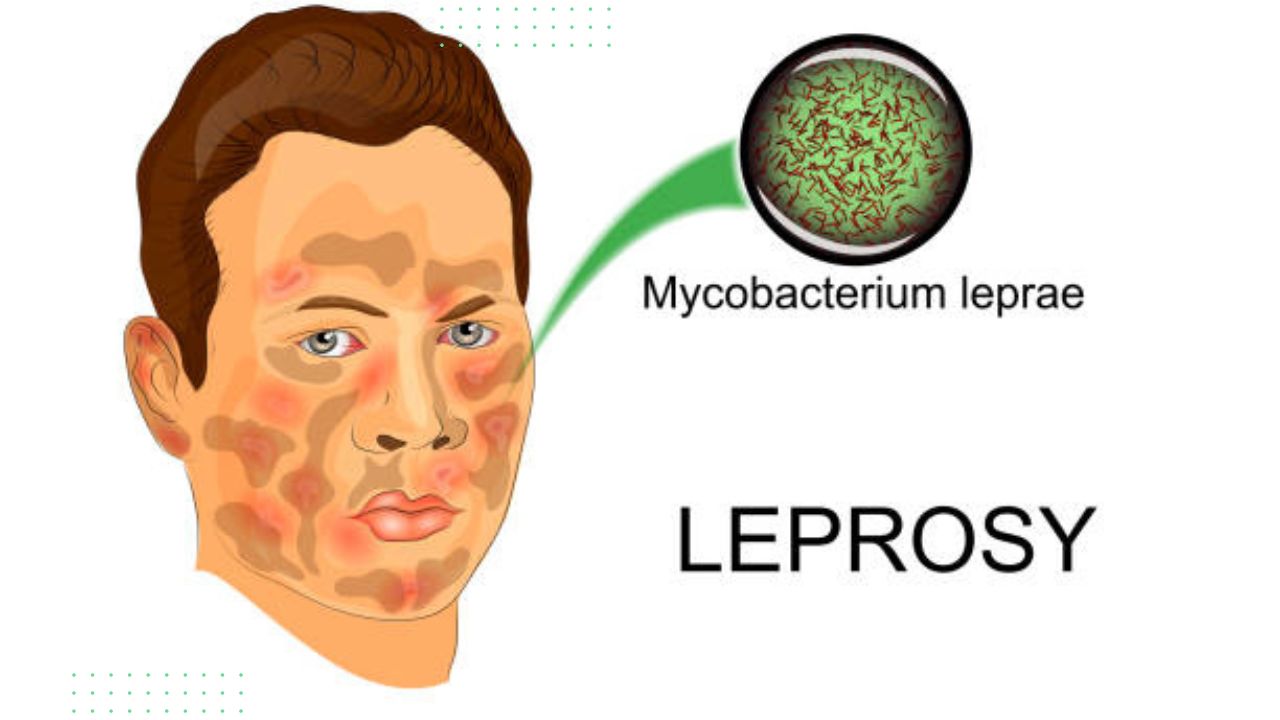
- Causes: Leprosy is caused by the bacterium Mycobacterium leprae.
- Risk Factors: Leprosy occurs particularly in tropical and subtropical countries with high population densities and low hygiene standards.
- Diagnosis: The diagnosis is made on the basis of the medical history, a physical examination and special examination methods for detecting the pathogen.
- Treatment: Leprosy is treated with a combination of different antibiotics.
- Prevention: When treating and caring for lepers, care should be taken to ensure adequate basic hygiene and the proper disposal of infectious materials.
What is leprosy?
Leprosy is a contagious bacterial disease also known as Hansen’s disease, Hansen’s disease or Hansen’s disease. It is caused by the Mycobacterium leprae and occurs worldwide. The bacteria destroy the skin and mucous membranes and attack the nerve cells.
The time between infection and the outbreak of the disease (incubation period) is up to 20 years in some cases, but on average three to seven years.
Countries particularly affected by leprosy include India, Brazil and Indonesia. Other countries affected include Nepal, the Republic of the Congo, Mozambique and Tanzania.
In general, the number of cases in Africa, America, Southeast Asia and the south-eastern Mediterranean has been declining since 2003. However, leprosy still exists and every year thousands of people worldwide are diagnosed with it – many of them children.
For example, 202,256 new infections were reported to the World Health Organization (WHO) in 2019, including 14,893 children under the age of 14.
Leprosy in the middle ages
Leprosy diseases were also very widespread in Europe in the Middle Ages. The disease was considered “God’s punishment”: The original name ” leprosy” probably comes from the fact that lepers had to live outside of human settlements (exposed).
What are the symptoms of leprosy?
Leprosy primarily affects the skin and nervous system. However, it may also affect the eyes, upper respiratory tract, bone marrow or testicles. There are different forms of leprosy, which manifest themselves through different symptoms.
Physicians distinguish between the following forms of leprosy:
Indeterminate leprosy is a very mild form of the disease, resulting in isolated, weakly pigmented (hypopigmented) patches of skin. In 75 percent of cases, these heal spontaneously.
Tuberculoid leprosy or nerve leprosy is the milder form of the disease. Skin changes are only isolated and sharply demarcated. The areas are less pigmented (hypopigmented) or reddened and do not itch. In this form of progression, the consequences of nerve damage are the typical symptoms of leprosy.
Tactile sensation (temperature, touch, and pain sensation) is lost. Since those affected do not feel pain early enough, they often injure themselves. The muscles atrophy, paralysis and sometimes serious deformations occur. The skin changes may heal on their own.
Lepromatous leprosy is a severe form of the infectious disease that occurs when the immune system is weak. Numerous tumor-like nodules appear on the skin, giving the face the appearance of a lion’s head (“Facies leontina”).
The mucous membranes of the nose, mouth and eyes may also be affected. Face, hands, feet and back are often mutilated. Loss of feeling in the affected areas only occurs later in the course of the disease. In the final stage, lepromatous leprosy spreads to the entire organism.
The so-called borderline forms of leprosy are mixed forms that combine different symptoms of the other forms.
Is leprosy curable?
Leprosy is a chronic disease of the skin, mucous membranes and nerve cells. With timely diagnosis and treatment, the prognosis is favorable.
However, if left untreated, it can lead to progressive and permanent damage to the skin, eyes, limbs and nerves.
Damage that has already occurred, such as mutilation or paralysis, cannot be reversed. About two to three million people worldwide are permanently affected by leprosy.
Leprosy: causes and risk factors
Leprosy is caused by the bacterium Mycobacterium leprae. The bacterium was discovered in 1873 by the Norwegian doctor Armauer Hansen as the cause of the infectious disease. Mycobacterium leprae is a less aggressive bacterium which, like the tuberculosis pathogen, lives in the infected host cells.
As a result, the immune system only fights the pathogen directly with defense cells (“cellular defense”) and a defense reaction via antibodies (“humoral defense”) hardly takes place. Only with massive and prolonged exposure to the bacterium does leprosy occur.
Leprosy occurs primarily in tropical and subtropical regions with high population densities and low hygienic standards.
Exactly how leprosy is transmitted has not yet been conclusively clarified. However, long-term, close contact with untreated lepers seems to play an important role. The infected excrete large amounts of the leprosy pathogen with nasal secretions or through the resulting skin ulcers.
The bacteria are then presumably transmitted from person to person via small skin wounds or the respiratory tract as droplet infection. Transmission of the pathogen during pregnancy to the unborn child is possible if the mother has leprosy.
Contrary to popular belief, leprosy is not a highly contagious disease! As a rule, it is therefore not necessary to isolate people with leprosy.
Investigations and diagnosis
An institute for infectious and tropical medicine is the right place to go if leprosy is suspected. The medical history is very important for the diagnosis.
The question of staying in leprosy risk areas in recent years is crucial, since leprosy has been eradicated in industrialized countries. During the physical examination, the doctor looks for typical skin changes, nerve changes and sensory disturbances.
Further investigations
Cultivation of the leprosy pathogen is extremely difficult and is therefore not carried out. However, the bacterium can be detected in smears of the skin or mucous membrane or in tissue samples (biopsies) under the microscope after special staining (detection of “acid-fast rods”).
Another possibility for diagnosis are so-called molecular-biological detection methods, for example the detection of the genome of Mycobacterium leprae by a polymerase chain reaction (PCR). This makes it possible to diagnose leprosy at an early stage. The method also serves to secure the diagnosis.
The lepromine test (Mitsuda reaction) is an antibody screening test that examines the body’s immune system. This test makes it possible to distinguish between tuberculoid and lepromatous leprosy.
Leprosy: treatment
The treatment of leprosy depends on the number of pathogens. A combination of different antibiotics is used. In tuberculoid leprosy, the active ingredients are usually dapsone and rifampicin, and in lepromatous leprosy clofazimine is also used.
The World Health Organization (WHO) recommends therapy for six months for so-called low-pathogen leprosy. On the other hand, pathogen-rich leprosy is treated with appropriate antibiotics for a period of at least twelve months.
In individual cases, the treatment is continued for even longer. It may then be necessary to resort to substitute medication (“reserve leprostatics”).
It often takes several years of therapy to completely heal the leprosy. Supportive exercise therapy helps to prevent paralysis caused by leprosy.
In addition, wound care is important. If the skin changes from leprosy have healed after successful therapy, rehabilitation measures are recommended. Your doctor will advise you on this.
Prevention
In order to avoid transmission of Mycobacterium leprae, basic hygiene and the proper disposal of infectious materials (e.g. nasal and wound secretions) must be ensured during the treatment and care of leprosy patients. It is recommended for persons who have been in contact with patients suffering from multibacillary leprosy to be monitored for clinical symptoms for at least five years.
Accordingly, close contacts should be tested for an infection every six months if possible. These examination intervals should be shortened if these people have additional risk factors, such as an immune deficiency caused by medication or infections.
Frequently asked questions and their answers
Is leprosy hereditary?
No, leprosy is not hereditary in the sense that it is not passed down from parent to child through genes. Leprosy is caused by an infection with the bacteria Mycobacterium leprae or Mycobacterium lepromatosis, which are spread through respiratory droplets when an infected person coughs or sneezes.
Is leprosy bacterial or viral?
Leprosy, also known as Hansen’s disease, is a bacterial infection caused by the bacteria Mycobacterium leprae or Mycobacterium lepromatosis. It is not a viral infection.
Mycobacterium leprae is a slow-growing, acid-fast bacillus (a type of bacteria) that mainly affects the skin and nerves. The bacteria can also affect other parts of the body, including the eyes, nose, and respiratory tract.
what is the early signs of leprosy?
The early signs of leprosy can vary depending on the type of leprosy and the individual. However, common early symptoms of leprosy include:
- Skin patches: The development of skin patches that are lighter or darker than the surrounding skin, and may or may not be numb.
- Numbness: Loss of sensation or numbness in the hands, feet, and other areas of the body.
- Muscle weakness: Weakness and paralysis of the muscles in the hands, feet, and face.
- Eye problems: Eye problems such as blurry vision, pain, and redness.
- Stuffy nose: Stuffy nose due to inflammation of the nasal passages.
- Thickened nerves: Enlarged nerves, especially around the elbows and knees.
What are leprosy drug?
Leprosy, also known as Hansen’s disease, is treated with a combination of antibiotics. The World Health Organization (WHO) recommends a multidrug therapy (MDT) regimen consisting of three antibiotics:
- Rifampicin: A bactericidal antibiotic that kills the bacteria that cause leprosy.
- Dapsone: A bacteriostatic antibiotic that stops the growth and multiplication of the bacteria that cause leprosy.
- Clofazimine: A bacteriostatic antibiotic that stops the growth and multiplication of the bacteria that cause leprosy.
The MDT regimen is typically given over a period of six months to two years, depending on the severity of the disease. The exact duration of treatment is determined by the healthcare provider based on the individual’s condition.
How many death leprosy are there?
According to the World Health Organization (WHO), in 2020, a total of 158 people died from leprosy worldwide. It’s worth noting that the number of deaths due to leprosy has been decreasing over the years, and many of these deaths occur in people who have advanced or untreated disease.
What is the last stage of leprosy?
The last stage of leprosy is also known as the advanced stage, and it can take many years to develop. During this stage, the bacteria that cause leprosy have caused significant damage to the skin, nerves, and other organs.
Symptoms of advanced leprosy may include:
- Loss of sensation in the skin: This can lead to injuries and infections that go unnoticed.
- Deformities: Leprosy can cause the bones and cartilage in the face, hands, and feet to become deformed, leading to claw-like hands or a “lion face” appearance.
- Blindness: Leprosy can cause eye damage that can lead to blindness.
- Chronic wounds: Leprosy can cause chronic ulcers and wounds that are difficult to heal.
- Nerve damage: Leprosy can cause nerve damage that leads to muscle weakness and paralysis.
Is leprosy Painful?
Leprosy, also known as Hansen’s disease, can cause pain in some individuals, especially in the advanced stages of the disease.
In the early stages of leprosy, a person may experience a loss of sensation or numbness in the affected area, which can make it difficult to feel pain. This can lead to injuries or infections that go unnoticed and cause further damage.
In the later stages of leprosy, the bacteria that cause the disease can damage the nerves, leading to chronic pain, muscle weakness, and paralysis. This nerve damage can also cause burning, tingling, or shooting pains.
Is leprosy fully treatable?
Yes, leprosy, is fully treatable with the proper medication and treatment. In fact, leprosy is one of the most curable infectious diseases.
The treatment for leprosy involves a combination of antibiotics, typically consisting of rifampicin, dapsone, and clofazimine, which are taken over a period of six months to two years, depending on the severity of the disease. This multi drug therapy (MDT) regimen is highly effective and has been used successfully for many years.
How do you get leprosy?
Leprosy is transmitted through prolonged and close contact with an infected person who has not received treatment. The bacteria that cause leprosy are transmitted through respiratory droplets, such as those expelled during coughing and sneezing. It is important to note that leprosy is not highly contagious, and most people who come into contact with an infected person do not develop the disease. In fact, over 95% of people have natural immunity to the bacteria that cause leprosy.
It is also believed that armadillos can transmit the disease to humans, although this is a rare occurrence.
Is leprosy contagious?
Leprosy, is contagious, but it is not highly contagious. The bacteria that cause leprosy are transmitted through respiratory droplets, such as those expelled during coughing and sneezing of an infected person who has not received treatment. Leprosy is not transmitted through casual contact, such as shaking hands, hugging, or sitting next to someone who has leprosy.
It’s important to note that most people who come into contact with an infected person do not develop the disease. In fact, over 95% of people have natural immunity to the bacteria that cause leprosy.