What is lung cancer?
Lung cancer – The lungs are two symmetrical, spongy organs located in the chest. Their function is to transfer the oxygen breathed into the bloodstream and to purify the blood of carbon dioxide produced by the body. With inspiration, the air enters the body through the nose and mouth and reaches the lungs passing through the trachea, a tube-like structure that divides into two branches, one directed to the right lung and one to the left lung. These two main branches divide into smaller ones called bronchi, which in turn divide into even smaller branches, the bronchioles. At the bottom of the bronchioles are the alveoli, cavities similar to “bags”, in which gaseous exchanges take place: through the many capillaries present in the alveoli.

The lung tumor , that may develop from the cells that constitute the bronchi, bronchioles and alveoli, can form a mass which can obstruct the air flow, or cause lung or bronchial bleeding. There is not just one type of lung cancer, but several forms of the disease. Furthermore, the lung can become the site of metastases of tumors affecting other organs (for example that of the breast).
How widespread is it?
The Italian Association of Cancer Registries estimates speak of 40,800 new diagnoses of lung cancer in 2020 (27,500 in men and 13,300 in women), which represent 14.1 percent of all cancer diagnoses in men and 7, 3 percent in women. In recent years there has been a moderate decrease in the incidence (number of new cases in a given period, for example a year) in men, but a significant increase in women: the explanation for these variations is the habit of smoking, which it fell in the male population and increased in the female population.
According to the data available today, one in 10 men and one in 35 women may develop lung cancer during their lifetime, while one in 11 men and one in 45 women are at risk of dying from the disease.
Lung cancer is one of the leading causes of death in industrialized countries, including Italy. In particular, in our country, this neoplasm is the first cause of death from cancer in men and the second in women, with almost 34,000 deaths in a year.
Who is at risk?
The most important risk factor for lung cancer is cigarette smoking: there is in fact a clear relationship between this habit and the disease, and this also applies to exposure to passive smoking. The more you’ve smoked (or the more smoke you’ve breathed in your life), the more likely you are to get sick. According to experts, both the amount of time one smoked and the number of cigarettes smoked matter. But the duration could be an even more important factor: if you start smoking a pack a day at a very young age and continue for the rest of your life, you can even get sick more than those who, however exposed to very high risk, smoke two. packages per day but for a shorter time. Quitting, on the other hand, leads to a strong reduction in risk.
In figures, the relative risk of smokers of lung cancer increases by about 14 times compared to non-smokers and even up to 20 times if they smoke more than 20 cigarettes a day.
Cigarette smoking is responsible for 8-9 out of 10 lung cancers, but also chemical carcinogens such as asbestos , radon and heavy metals are risk factors for this disease, especially for that part of the population that comes to contact with these substances for work reasons: in this case we speak of occupational exposure.
Air pollution , cases of lung cancer in the family (especially in parents or siblings) and previous lung diseases or radiotherapy treatments that have affected the lungs (perhaps due to previous lymphoma) also increase the risk of getting sick .
The data that explain at the molecular level the mechanisms that lead to the development of lung cancer are increasingly precise : among the genes involved we remember – just to name a few – the tumor suppressors p53 and p16 (genes that “keep the tumor at bay”) and ‘ oncogene K-RAS (a disease- promoting gene ) for non- small cell cancer and p53 and RB1 for small cell cancer.
Types of lung cancer
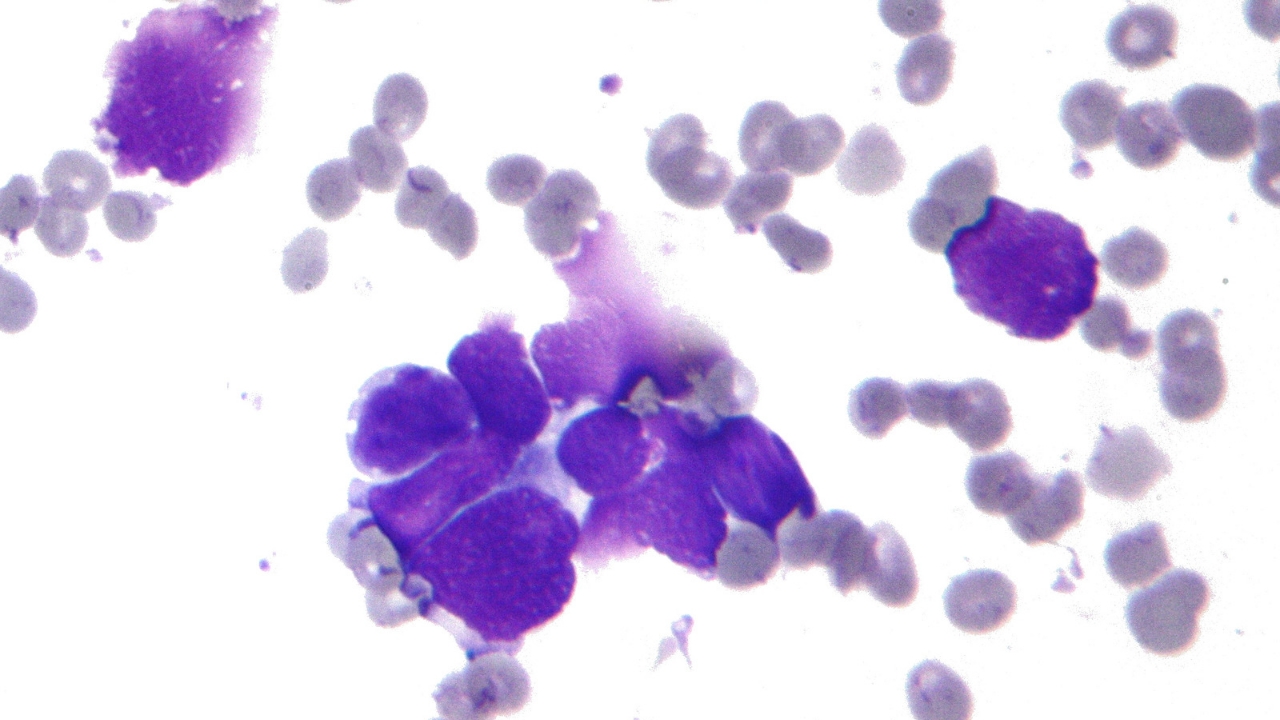
From a clinical point of view it is customary to distinguish two main types of lung cancer which together represent over 95 percent of all neoplasms that affect these organs: small cell lung cancer (also called microcytoma, a category to which the 10-15 percent of cases) and non-small cell lung cancer (the remaining about 85 percent), both of which originate from the epithelial tissue lining the lung structures.
The small cell lung cancer, or small cell (in scientific texts often abbreviated as SCLC, English small-cell lung cancer), is developed in the larger diameter bronchi, is made from small cells and usually occurs in smokers, while it is very rare in those who have never smoked. Its prognosis is worse than that of non-small cell cancer also because the disease spreads very quickly to other organs.
The cancer non-small cell (in scientific texts often abbreviated as NSCLC, from the English “non-small-cell lung cancer”) is in turn divided into three main types:
- the cancer squamous cell (also called squamous cell carcinoma or squamous cell) represents 25-30 percent of the cases and was born in the airways of medium-caliber from the transformation of the ‘epithelium lining the bronchi, caused by cigarette smoke. It is the lung cancer with the best prognosis.
- adenocarcinoma accounts for approximately 60 per cent of the cases and is localized, unlike the previous ones, in most peripheral seat, namely in the bronchi level of smaller diameter. It is the most frequent lung cancer among those who have never smoked and is sometimes due to the presence of lung scars (for example from old tuberculous infections or pleurisy).
- The large cell carcinoma is less frequent (10 per cent) and can appear in different areas of the lung. It generally tends to grow and spread quite rapidly.
In the remaining 5 percent of cases the tumor does not originate from the epithelium but from different tissues, such as endocrine tissues (in this case we are talking about lung carcinoid of neuroendocrine origin) or lymphatic (in this case it is lung lymphoma ).
Symptoms of lung cancer
Lung cancer in many cases remains asymptomatic in the early stages, in fact sometimes the disease is diagnosed during tests carried out for other reasons. When present, the most common symptoms of lung cancer are continuous cough that does not go away or even gets worse over time, hoarseness, blood in the phlegm, shortness of breath, chest pain that increases in the case of a cough or deep breath, loss of weight and appetite , fatigue , respiratory infections (bronchitis or pneumonia) that are frequent or return after treatment.
The tumor can also spread by contiguity to nearby structures (the pleura that lines the lungs, chest wall and diaphragm), by lymphatic route to the lymph nodes or through the bloodstream. Almost all organs can be affected by metastases – liver, brain, adrenal glands, bones, kidneys, pancreas, spleen, and skin – resulting in specific symptoms such as bone pain and jaundice, neurological symptoms such as headache or dizziness, and visible nodules. on the skin.
Prevention of lung cancer
To prevent lung cancer, the first and most important step is undoubtedly to avoid smoking .
In the case of non-smokers it is almost impossible to completely escape passive smoking, but it is good practice to ask on every occasion that the prohibitions imposed in public and work places are respected, especially in the presence of children.
Regarding the risk factors related to the profession, it is important to always use all protective measures in the workplace in order to minimize risks and work safely.
In everyday life, to prevent the disease it is good to do regular physical exercise and introduce lots of fruits and vegetables in the diet, rich in vitamins and other elements that can help the lungs to stay healthy.
Although there are numerous researches in this area, there is still no agreement among experts on the advisability of subjecting apparently healthy people to ” screening ” (ie periodic examinations for the early diagnosis of the population), without any symptoms or signs of disease. The reason is that simple diagnostic tests, such as chest X-rays or sputum cytology, do not always allow to identify a possible tumor, much less early.
Several studies conducted with high-risk, heavy smokers with many years of smoking, suggest that spiral computed tomography ( CT ) of the lungs could be useful in detecting small lung cancers in asymptomatic patients, saving years of life. However, these tests also have some risks: the lungs are very sensitive to radiation and frequent tests of this type could cause tissue damage. Furthermore, these tests can also detect pulmonary alterations that look like but are not necessarily tumors: a result that requires a biopsy to be clarified , that is an invasive sampling of tissue.pulmonary which in turn carries risks. Population lung screening can also cause problems with overdiagnosis, that is, with the detection of lung cancers that may never become life- threatening for a person’s life, but in such cases patients would be subjected to unnecessary treatments for lung cancer. , with the related side effects.
To mitigate these problems and identify patients who would be most likely to benefit from spiral CT screening, research is being carried out on other possible diagnostic tools that could possibly be combined with this examination, such as analysis of respiratory gases and markers present in the biological samples. In particular, some microRNAs – small fragments of genetic material – have been identified that could be useful in determining the risk of developing lung cancer, even before there are detectable nodules.
However, the studies will still take some time before routine screening for early lung cancer can be proposed by researchers and approved for wide use by regulatory authorities.
Diagnosis of lung cancer
In the presence of suspicious symptoms it is important to contact your GP who, after a thorough examination in which he will evaluate all the signs and symptoms, may prescribe further in-depth examinations such as a chest X-ray . Further investigations may include the use of CT and PET , but to arrive at a certain diagnosis it is necessary to carry out a biopsy – removal of a fragment of tumor tissue – and the subsequent histological examination , i.e. the study of the fragment taken under the microscope. To get a more accurate picture of the situation, the doctor may prescribe bronchoscopy, with which it is possible to visualize the inside of the bronchi thanks to a thin tube inserted through the mouth, also useful for performing tissue sampling without resorting to surgery.
The evaluation of lung function , or how the lungs work, is essential if you plan to resort to surgery to remove part of the lung. During the analysis of the tissue samples taken, it is now possible to determine the presence of particular molecules on cancer cells that may represent the targets for the so-called “targeted drugs”, thus helping doctors to decide which treatment to use for the treatment of each individual. patient.
Evolution
Non-small cell lung cancers are classified into four stages of increasing severity, denoted by Roman numerals I to IV. For staging (the process that allows you to assign a stage to the evolution of the disease) the so-called TNM system is used. Parameter T describes the size of the primary tumor (i.e. the one that appeared first in the event that the disease has spread to other sites), parameter N indicates any involvement of the lymph nodes and finally parameter M refers to presence or absence of distant metastases.
Small cell cancer is traditionally classified into two stages, limited or extensive .
In Italy, only 16.4 percent of men and 22.7 percent of women with lung cancer are alive 5 years after diagnosis. The survival is adversely affected by the fact that the disease is almost always diagnosed when the cancer is at an advanced stage and that the drug therapies used in the advanced stages of the disease often give benefits only transient.
How to cure
The therapeutic approach changes according to the patient’s condition and stage, the molecular characteristics and above all the histological type of the tumor.
Non-small cell tumor

In non-small cell cancer, surgery is the most common therapy of choice, unless distant metastases are already present. Since portions of the lung are removed during surgery, it is important to evaluate the patient’s lung function before surgery to be sure there will be no breathing problems.
The radiation therapy is used alone or in combination with chemotherapy in cases where it is not possible to proceed with surgery, due to the characteristics of the tumor or the patient’s health status.
Pharmacological therapies are used in patients already operated on at high risk of relapse and with advanced disease or who have developed metastases. The chemotherapy standard consists of the administration of cisplatin or carboplatin in combination with gemcitabine, etoposide, pemetrexed, docetaxel, paclitaxel or vinorelbine. Radiotherapy and chemotherapy can be used before surgery (neoadjuvant therapy) to reduce the size of the tumor or after surgery (adjuvant therapy) to eliminate any remaining cancer cells.
Molecularly targeted therapies are used whenever possible . Patients with mutations in the gene encoding EGFR, a growth factor receptor involved in cell proliferation, respond to tyrosine kinase inhibitors such as gefitinib, erlotinib, afatinib and osimertinib. These mutations have been found in about 10-15 percent of patients diagnosed in Italy. A minority of patients (3-7 percent) who instead have an alteration of the gene that codes for ALK, a proteinwhich produces a growth stimulus for the cells, responds to treatment with ALK inhibitors (crizotinib, alectinib, ceritinib, brigatinib and lorlatinib). In non-squamous tumors, bevacizumab and nintedanib, drugs that block angiogenesis, ie the formation of new blood vessels , can also be used in combination with chemotherapy .
Lung cancer treatment has been partially revolutionized by immunotherapy. Immunological checkpoint inhibitors interfere with a mechanism used by the tumor to prevent immune cells from activating and stimulate the antitumor response. Monoclonal antibodies that recognize PD-1 (nivolumab, pembrolizumab) or PD-L1 (atezolizumab, durvalumab) proteins, alone or in combination with chemotherapy, have become key drugs in the treatment of non-small cell cancer.
Finally, in specific cases, it is possible to resort to local treatments such as stereotaxic radiotherapy , radiofrequency ablation (to destroy the tumor with heat), photodynamic therapy (a drug is injected which is then activated thanks to the light of a bronchoscope and destroys cancer cells) and laser therapy.
Small cell tumor
The most used treatment for this type of cancer is chemotherapy, a choice linked to the fact that in most cases, metastases in other organs are already present at the time of diagnosis. Standard therapy consists of the administration of cisplatin (or carboplatin) and etoposide. Other drugs used can be doxorubicin, cyclophosphamide and topotecan. Some studies have suggested that small cell cancer patients may also benefit from immunotherapy with immunological checkpoint inhibitors combined with chemotherapy.
In small cell cancer, radiation therapy is used in conjunction with chemotherapy or after chemo to eliminate any remaining cancer cells. It is often used in the brain to reduce the risk of metastases in this organ (very common) or for palliative purposes, that is, to reduce symptoms in more advanced cases. Surgery is indicated only in selected cases and is performed very rarely.