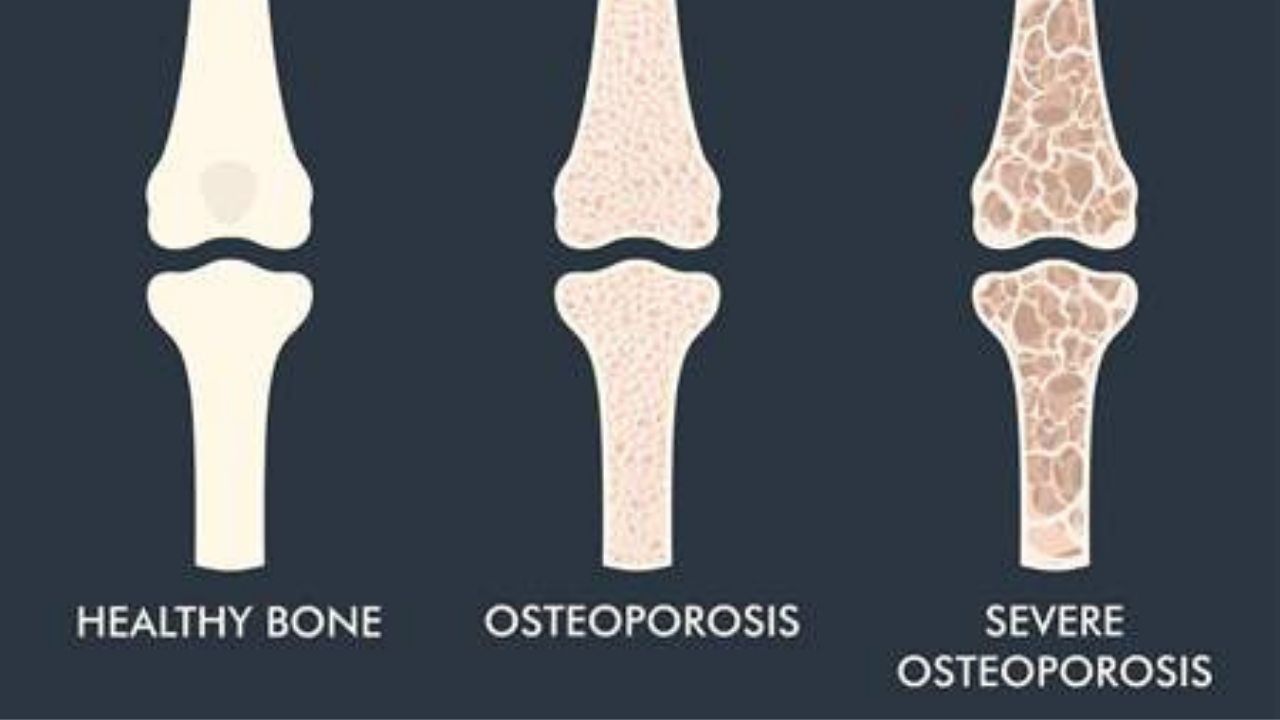
Osteoporosis is a systemic disease of the skeleton, characterized by a decrease in bone mass (BMD) and a violation of its quality (microarchitectonics), which lead to fragility of bones and subsequent fractures with minor trauma (for example, falling from a height of their own growth).
The most common sites for osteoporotic fractures are a fracture of the radius at a “typical site”, namely the wrist, a fracture of the proximal femur, or femoral neck, and compression fractures of the vertebrae. It is these consequences of the course of osteoporosis that lead to disability.
Types of osteoporosis:
- Primary osteoporosis:
(a) postmenopausal (type I)
(b) senile (type II) (elderly people)
(c) juvenile (children)
(d) idiopathic (the reason is not clear)
- Secondary osteoporosis:
- diseases of the endocrine system: disease or Itsenko-Cushing’s syndrome. thyrotoxicosis, hypogonadism, hyperparathyroidism, diabetes mellitus, etc.
- rheumatic diseases: Rheumatoid arthritis, Systemic lupus erythematosus, ankylosing spondylitis, etc.
- diseases of the digestive system: conditions after resection of the stomach, malabsorption, chronic liver disease.
- kidney disease: chronic renal failure, renal tubular acidosis, Fanconi syndrome.
- blood diseases: myeloma, thalassemia, leukemia, lymphoma, etc.
- other diseases and conditions: immobilization, oophorectomy, chronic obstructive pulmonary disease, alcoholism, anorexia nervosa, nutritional disorders, organ transplantation
- genetic disorders: osteogenesis imperfecta, Morphan’s syndrome, homocystinuria and lysinuria, etc.
- drugs: glucocorticoids, immunosuppressants, gonadotropin-releasing hormone agonists, antacids containing aluminum, thyroid hormones.
The main risk factors for osteoporosis and bone fractures are:
- age over 65,
- female,
- Caucasian race,
- previous fractures
- low mineral density,
- tendency to fall,
- heredity (family history of osteoporosis),
- hypogonodism in men and women,
- decreased creatinine clearance and / or glomerular filtration rate,
- body mass index less than 20 kg / m2 and / or body mass less than 57 kg,
- systemic intake of glucocorticoids for more than 3 months,
- smoking,
- insufficient calcium intake,
- alcohol abuse
- low physical activity,
- prolonged immobilization.
The clinical picture of fractures:
Osteoporosis is called a “silent epidemic”. This means that if the patient does not have a fracture, then there are no symptoms. For fractures, they can be different:
- chronic or new-onset back pain (it should be recalled that back pain can be found in a number of other diseases and pathological conditions, besides osteoporosis),
- decrease in height by 2 cm or more in 1-3 years or by 4 cm or more compared to growth at 25 years old (reflects a decrease in the height of the vertebrae during compression),
- the distance between the back of the head and the wall is more than 5 cm (reflects the presence of thoracic kyphosis),
- the distance between the lower ribs and the wing of the ilium is 2 x fingers or less (reflects the shortening of the spinal trunk due to compression of the vertebrae).
As mentioned above, BACK PAIN is not a specific symptom, therefore, it is possible to suspect an osteoporotic vertebral fracture if there is a combination with at least one of the following signs:
- onset of pain at the age of over 50,
- an indication of a fall from a height of one’s own growth or lifting weights,
- connection with trauma,
- previous fractures
- age over 55,
- long-term use of glucocorticoids.
Diagnosis of osteoporosis
Densitometry is the main instrumental method for diagnosing osteoporosis, measuring bone mineral density by X-ray densitometry (DXA), preferably along the proximal femur and spine. If axial DXA is impossible, peripheral DXA can be used at the level of the distal third of the forearm bones.
Indications for assessing BMD at the initial examination:
1. Women aged 65 and over.
2. Postmenopausal women under the age of 65 with fracture risk factors.
3. Men aged 70 and over.
4. Men under 70 with fracture risk factors.
5. Persons who have suffered a low-energy fracture after 40 years.
6. Persons with diseases or conditions associated with low BMD.
7. Persons taking medications associated with low BMD.
X-ray examination:
Should be carried out to diagnose fractures of the bones of the peripheral skeleton and vertebrae.
Laboratory tests:
The goal is to carry out differential diagnostics with other diseases of the skeleton and to identify contraindications to the appointment of drug therapy.
- general clinical blood test,
- calcium and phosphorus in blood serum,
- creatinine clearance,
- alkaline phosphatase,
- total protein and protein fractions by electrophoresis in patients with vertebral fractures,
- parahormone,
- 25 – (OH) – D3.
Preventive measures:
- Correction of nutrition (foods rich in calcium and vitamin D)
- Quitting smoking and alcohol abuse
- Measures to reduce the risk of falls:
- vision correction
- assessing and changing the home environment (making it safer)
- teaching the correct stereotype of movements
- learning to use a cane
- stable shoes with low heels
- physical exercises for coordination and balance training
Treatment methods for osteoporosis:
Non-drug therapy for osteoporosis:
1. Walking and exercise (weight bearing exercise, strength exercise and balance training)
2. Jumping and running are contraindicated.
3. Quitting smoking and alcohol abuse
4. Wearing rigid and semi-rigid corsets to reduce the severity of pain after a vertebral fracture (no more than 6 hours per day). ps: long-term wearing of a corset can lead to weakness of the back muscles and, as a result, to poor long-term results.
5. Constant wearing of hip protectors by patients with a high risk of developing a hip fracture and risk factors for falls.
6. It is possible to use kyphoplasty and vertebroplasty to reduce pain, correct posture in patients with vertebral fractures and chronic back pain.
7. Manual therapy for osteoporosis is contraindicated !
Drug therapy:
Calcium and vitamin D preparations: Treatment with any drug of pathogenetic action should be accompanied by the appointment of adequate doses of calcium (1000-1200 mg / day, taking into account food) and vitamin D up to 2000 IU per day.
Pathogenetic drugs:.
1. Drugs that stop the destruction of bone tissue:
– bisphosphonates (duration of treatment from 3 to 5 years. Sometimes over 5 years.
– Denosumab (duration of treatment up to 10 years).
2. A drug that stimulates bone formation:
– Teriparatide (duration of treatment up to 2 years).
