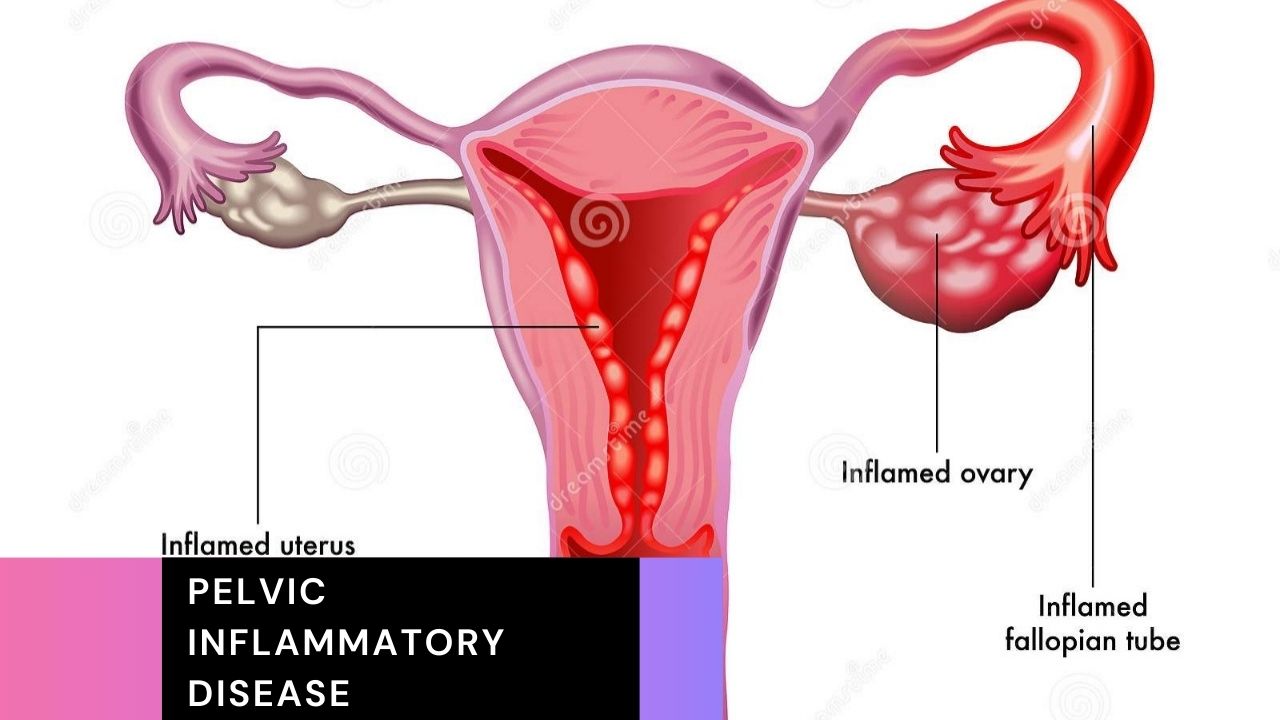
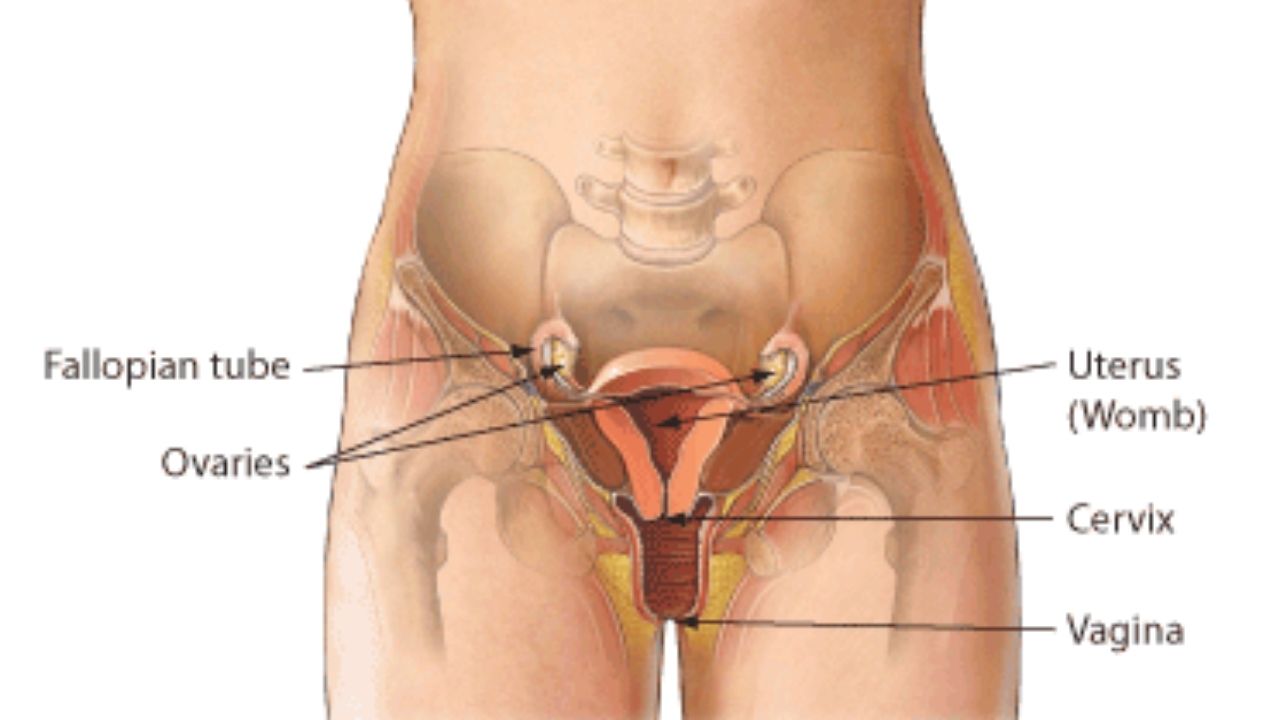
Pelvic inflammation is a bacterial infection of the upper female genital organs (cervix, fallopian tubes, uterus and ovaries). In this article we will explain about pelvic inflammatory disease, such as symptoms, causes, prevention, treatment and how pelvic inflammatory disease is diagnosed?.
What is pelvic inflammatory disease?
Pelvic inflammation, also known as PID, is a health condition that affects different parts of the female reproductive system, including the ovaries, fallopian tubes, uterus, and genital tract. The main cause of this condition is usually bacterial infection, and it is not uncommon for multiple strains of bacteria to be present at the same time.
- Pelvic inflammation is usually transmitted during sex with an infected partner.
- Usually women experience lower abdominal pain, vaginal discharge, and irregular vaginal bleeding.
- Diagnosis is based on symptoms, analysis of secretions from the cervix and vagina, and sometimes an ultrasound.
- The risk of infection decreases if you have only one partner and if you use condoms.
- The infection is fought with antibiotics.
A pelvic inflammation can be one of the following infections:
- Cervix, i.e. the lower, narrow part of the uterus that opens into the vagina (cervicitis).
- Lining of the womb (endometritis).
- Eileiter (Salpingitis).
- A combination of the above infections.
If the infection is severe, the following can happen:
- PID can spread to the ovaries.
- Lead to an accumulation of pus in the fallopian tubes (tubo-ovarian abscess).
In about a third of women with pelvic inflammation, the infection will develop again.
Pelvic inflammation mostly occurs in sexually active women of childbearing age. It rarely occurs in girls before the first menstrual period (menarche) or in women during pregnancy or after menopause. The risks are higher for the following women:
- Women who are sexually active and younger than 35.
- A woman whose partner does not use a condom.
- Women with many or new sex partners.
- Women with a sexually transmitted disease or bacterial vaginosis.
The onset of the disease is characterized by a range of symptoms, including pelvic pain, painful urination, and changes in menstrual cycles, such as bleeding between periods or more intense periods.
In some cases, these symptoms can go unnoticed for a long time. If left untreated, pelvic inflammatory disease can lead to additional complications, including abscesses, chronic pelvic pain, and in some cases even infertility.
Typically, to diagnose the condition, a medical professional needs to do a pelvic exam and then do a laboratory analysis. Simple and painless swab samples are mainly used for further analysis.
In addition, the doctor can request additional diagnostic procedures, e.g. B. Take blood or urine samples or perform an ultrasound scan. In any case, all the diagnostic methods used are completely painless and safe.
If PID is detected early, it can easily be treated with antibiotics. However, more serious cases or cases that were only discovered after the infection had progressed may need to be hospitalized to receive proper treatment.
What are the symptoms of pelvic inflammatory disease?
The symptoms of PID are known, but they can still be mistaken for sexually transmitted diseases or other urinary problems. In addition, when the symptoms are subtle, many women may miss them completely. They include:
- Pain in the lower abdomen.
- Fever.
- Vaginal discharge.
- Heavier and more intense periods.
- Bleeding after sex or between periods.
- Pain and burning sensation when urinating.
- Changes in the color and consistency of the discharge.
- Nausea and vomiting (in severe or advanced infection).
Causes of pelvic inflammatory disease
Pelvic inflammation is usually caused by bacteria in the vagina. In most cases, the bacteria are transmitted during sexual intercourse with a partner who has a sexually transmitted disease. The most common sexually transmitted bacteria are:
- Neisseria gonorrhoeae, also known as gonococcus or gonococci, which causes gonorrhea.
- Chlamydia trachomatis, which causes chlamydial infections.
- Mycoplasma genitalium.
As mentioned briefly, PID is caused by a bacterial infection and there are several strains that can be responsible for causing the disease to break out. These can be bacteria that cause STIs, such as chlamydia or gonorrhea.
In a majority of diagnosed cases, pelvic inflammatory disease is caused by the simultaneous presence of several types of bacteria in the female reproductive system.
However, Chlamydia trachomatis, the strain responsible for genital chlamydia, and Neisseria gonorrhoeae, which cause gonorrhea, are present in a significant proportion of those affected, implying a strong correlation between STIs and PID.
According to statistical studies, around a quarter of all diagnosed PID cases can be traced back to untreated chlamydia or gonorrhea. In contrast, official CDC information states that these STIs could be responsible for 33% to 50% of PID cases.
Regardless of which type of bacteria is the culprit, this condition is always caused by the migration of microbes from the vagina past the cervix to the upper genital tract. These microorganisms can be harmless and natural in the vagina, but become problematic once they are introduced into other parts of the reproductive system. This underscores the fact that while STIs are often to blame, this is not true in all cases.
Infection can also occur if the cervix is damaged during childbirth or a miscarriage. There are also certain medical procedures that may require the cervix to be opened (e.g. to put in a birth control coil), which is another risk factor.
In addition, anything that causes bacterial vaginosis by disrupting the balance of the vaginal fauna (e.g., showering) can also trigger PID.
The most common preventable cause of infertility is pelvic infection.
Who is at risk of developing PID?
Women who are sexually active are at significantly higher risk, and so are women who have had a history of pelvic inflammatory disease. Despite the clear presence of these risk groups, any woman can be affected, regardless of whether she is sexually active or not.
Public Health England conducted a study in 2015 that found that the highest rate of diagnosis in the GP range was in women between 20 and 24 years old, while in the hospital the highest rate of diagnosis was in those aged 35 to 44 years old of 15- to 44-year-olds give PHE 176 diagnoses per 100,000 women in primary care and 241 further cases per 100,000 women in hospital.
Can PID cause further complications?
There are several potentially serious health conditions and complications that can result from untreated pelvic inflammation. These include:
- Recurrent PID, caused by the primary infection that damages the reproductive organs, making them more susceptible to secondary infections.
- Long-term pelvic pain.
- Abscesses in the ovaries or fallopian tubes.
- Infertility in cases where the infection causes lasting damage to the fallopian tubes (this occurs in about 1 in 10 PID cases).
- Ectopic pregnancy (pregnancy that develops outside of the uterus, most typically in the fallopian tubes).
As with most health conditions, the likelihood of complications is dramatically reduced with early diagnosis and treatment of PID.
Sometimes the infected fallopian tubes close up. They can then swell because secretions build up. Women feel pressure or have chronic pain in the lower abdomen.
The peritonitis occurs when the infection spreads to the membrane lining the abdominal cavity and covers the abdominal organs. Such peritonitis can cause sudden or gradual severe pain throughout the abdomen.
The Fitz-Hugh Curtis syndrome occurs when the infection of the fallopian tubes to gonorrhea and chlamydia infection back and propagates to the tissue around the liver. Such an infection can cause pain in the upper right abdomen. The pain is similar to that of a gallbladder infection or gallstones.
15 percent of women with an infection of the fallopian tubes will develop an abscess in the fallopian tubes or ovaries , especially if the infection has been long-lasting. When the abscess ruptures, the pus spreads throughout the abdominal cavity, causing peritonitis. This triggers severe pain in the lower abdomen and, shortly afterwards, nausea, vomiting and an abrupt drop in blood pressure (circulatory shock). The infection can spread to the blood (blood poisoning or sepsis) and be fatal. It is a medical emergency.
Adhesions are unusual strands of scar tissue. They can develop when a pus-like fluid forms in a pelvic inflammation. This fluid irritates the tissues and leads to the formation of strands of scar tissue in the reproductive organs or between organs in the abdomen.
Infertility and chronic abdominal pain are the result. The longer, more severe the inflammation, and the more often it returns, the greater the risk of infertility and other complications. The risk increases with each new infection.
An ectopic pregnancy (a form of ectopic pregnancy) in women with pelvic inflammatory 6- to 10 times more likely. The fetus does not grow in the uterus, but in the fallopian tube. Such a pregnancy is life-threatening for the woman and the fetus cannot survive.
How pelvic inflammatory disease is diagnosed?

If you also want to know how pelvic inflammatory disease is diagnosed then you have come to the right place.
The doctor will do various tests to see if you have PID and to rule out other possible conditions. The most common methods used by medical professionals are:
- Gynecological examination (usually the first stage of the diagnostic process)
- Cervical swab (to check for possible chlamydia or gonorrhea)
- Urine and blood tests (to confirm the diagnosis and rule out other causes)
- Ultrasound and pregnancy tests (as above)
- Laparoscopy – a procedure when small incisions are made in the abdomen and a small camera is used to check the area for signs of inflammation (very rarely used method).
Doctors suspect pelvic inflammation if women have abdominal pain or an unexplained discharge from the vagina, especially if they are of childbearing age or if the discharge is purulent.
A physical exam, including a pelvic examination, will be done. Pelvic pain during the pelvic examination supports the diagnosis.
A sample is usually taken from the cervix with a swab and tested to see if the woman has gonorrhea or chlamydial infection. Even if these tests do not reveal gonorrhea or chlamydial infection, pelvic inflammation may still be present.
A pregnancy test will be done to see if the woman may have an ectopic pregnancy, which would be causing the symptoms. Other symptoms and results from laboratory tests will help confirm the diagnosis.
A pelvic ultrasound is done if the pain prevents an adequate physical examination or if more information is needed. Abscesses in the fallopian tubes or ovaries and an ectopic pregnancy can be detected.
If the diagnosis is still not certain or the woman does not respond to treatment, the doctor may insert a viewing tube (laparoscope) through a small incision near the navel to examine the inside of the abdomen and obtain a sample of fluid for further testing. This procedure can usually confirm or rule out pelvic inflammation.
Treatment of pelvic inflammatory disease
- Antibiotics.
- If necessary, the drainage of an abscess.
Usually, antibiotics for gonorrhea and chlamydial infection are given by mouth or injected into a muscle as soon as possible. Immediate treatment of PID is necessary to avoid serious complications. If necessary, antibiotics are changed after the test results are available.
Most women are treated at home with oral antibiotics. Hospitalization is required in some conditions. Which can be include:
- The woman has severe symptoms or a high fever.
- The woman is pregnant.
- An abscess is suspected.
- The woman vomits and cannot take antibiotics orally at home.
- Doctors cannot confirm a diagnosis of pelvic inflammation or rule out conditions that may require surgery (such as appendicitis).
In the hospital, antibiotics are given intravenously.
Abscesses that do not heal despite treatment with antibiotics can be drained. A needle can often be used. It will be inserted through a small incision in the skin and an imaging test such as An ultrasound or computed tomography (CT) scan is used to guide the needle into the abscess. If an abscess ruptures, emergency surgery is required.
If diagnosed early, PID can be treated with an antibiotic regimen, which usually lasts for 14 days.
You will be given a mixture of antibiotics to cover the most likely infections, and often an injection and pills.
It is important to complete the entire course of PID treatment and not have sexual intercourse during this time to ensure that the PID infection is cleared.
Your youngest sexual partners will also need to be tested and treated to prevent the infection from returning or being passed on to others.
Women should not have sexual intercourse until antibiotic treatment is completed and the infection has completely resolved.
All recent sexual partners should be examined for possible infection and treated if in doubt. If pelvic inflammation is diagnosed and treated promptly, a cure is more likely.
Complications of PID
The fallopian tubes can become scarred and narrowed when affected by PID. This can make it difficult for eggs to get from the ovaries to the womb.
This can then increase your chances of conceiving in the fallopian tubes instead of the uterus (ectopic pregnancy) in the future and may render some women stother.
It is estimated that about 1 in 10 women with PID become infertile as a result of the condition. Women who have delayed treatment or who have had repeated episodes of PID are at higher risk.
But most women being treated for PID can still get pregnant without any problems.
Prevention of PID
The most important preventive measure to avoid pelvic inflammatory disease is to use condoms during sexual intercourse. Condoms are the best way to prevent the spread of sexually transmitted infections (STIs).
Individuals diagnosed with an STI should contact their previous sex partners so that they can also be tested and treated if necessary.
Outlook
Most people recover well from treatment and the infection does not cause long-term discomfort.
However, if the infection was not treated, or if a person becomes infected again after treatment, complications are more likely to occur.
These may include scarring of the uterus or fallopian tubes, difficulty getting pregnant, pregnancies outside the uterus (extrauterine pregnancies), and prolonged pelvic pain.