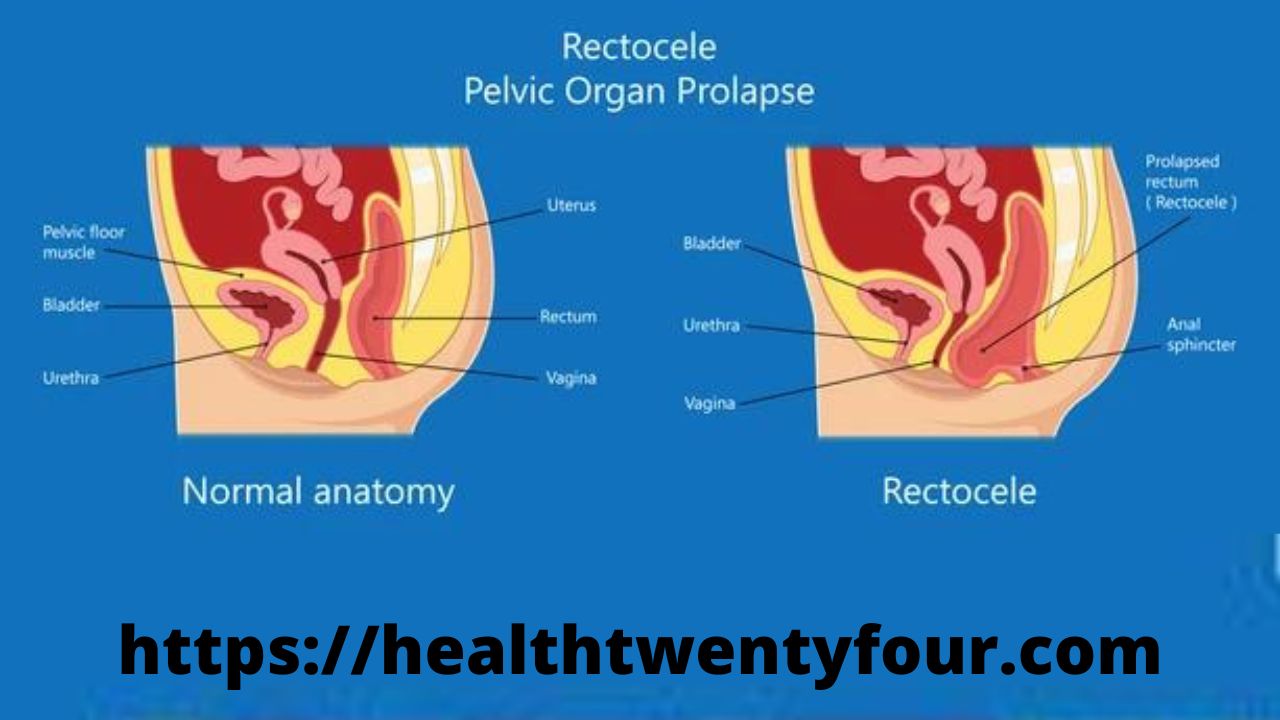
Posterior vaginal prolapse occurs when the thin wall of tissue that separates the rectum from the vagina weakens, causing the vaginal wall to protrude. Posterior vaginal prolapse is also known as a rectocele.
Childbirth and other processes that put pressure on the pelvic tissues can lead to posterior vaginal prolapse. A mild prolapse may not cause any signs or symptoms.
If the posterior vaginal prolapse is large, it can create a noticeable bulge of tissue through the vaginal opening. While this lump can be uncomfortable, it is rarely painful.
If necessary, there are self-care measures and other non-surgical options that are often effective. Severe posterior vaginal prolapse may require surgery.
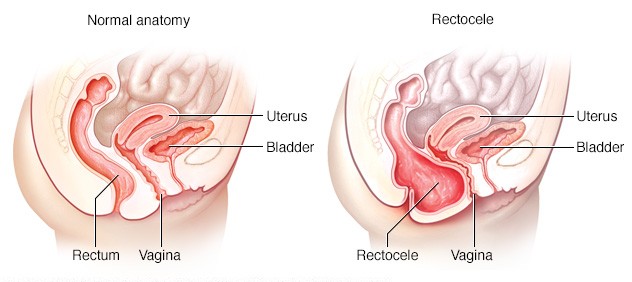
Posterior vaginal prolapse, also known as a “rectocele,” occurs when the wall of fibrous tissue that separates the rectum from the vagina weakens. When this happens, the tissues or structures just behind the vaginal wall—in this case, the rectum—may bulge into the vagina.
Symptoms
A mild posterior vaginal prolapse (rectocele) may not cause any signs or symptoms.
Otherwise, you might notice the following:
- A bulge of soft tissue in the vagina that may protrude from the vaginal opening.
- Difficulty defecating.
- Sensation of rectal pressure or of having the rectum full.
- Feeling that the rectum has not emptied completely after a bowel movement.
- Sexual concerns, such as feeling embarrassed or a feeling of loosened vaginal tissue tone.
Many women with posterior vaginal prolapse also have prolapse of other pelvic organs, such as the bladder, uterus, or upper vagina in women who have had surgery to remove the uterus (hysterectomy).
When you should see a doctor
Posterior vaginal prolapse is common, even in women who have not had children. In fact, you may not even know you have posterior vaginal prolapse.
However, in moderate to severe cases, posterior vaginal prolapse can be bothersome or uncomfortable. Consult the doctor in the following cases:
- If you have an uncomfortable bulge of tissue protruding from the vaginal opening.
- Treatment for constipation fails to produce soft, easy-to-pass stools three times a day to three times a week.
Causes
Posterior vaginal prolapse is caused by pressure on the pelvic floor. Causes of increased pelvic floor pressure include:
- Chronic constipation or pressure when having a bowel movement.
- Bronchitis or chronic cough.
- Repeatedly lifting heavy objects.
- Overweight or obesity.
Pregnancy and childbirth
The muscles, ligaments, and connective tissue that support the vagina are stretched and weakened during pregnancy, labor, and delivery. The more pregnancies you have, the greater the chance of developing posterior vaginal prolapse.
Women who have only had cesarean deliveries are less likely to develop posterior vaginal prolapse, but can still do so.
Risk factor’s
Factors that may increase the risk of posterior vaginal prolapse include:
- Genetics. Some women are born with weaker connective tissues in the pelvic area, making them naturally more prone to posterior vaginal prolapse.
- Birth. If you gave birth to multiple children vaginally, you are at higher risk of posterior vaginal prolapse. If you had any tears in the tissue between the vaginal opening and the anus (perineal tear) or had incisions made to enlarge the opening of the vagina (episiotomies) during childbirth, you may also be at higher risk.
- Aging. As you age, you naturally lose muscle mass, elasticity, and nerve function, causing muscles to stretch or weaken.
- Obesity. Excess body weight puts pressure on the pelvic floor tissues.
Prevention
To reduce the risk of worsening posterior vaginal prolapse, try the following:
- Perform Kegel exercises regularly. These exercises can strengthen your pelvic floor muscles, which is especially important after having a baby.
- Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods like fruits, vegetables, beans, and whole grains.
- Lift objects correctly and avoid heavy lifting. When lifting objects, use your legs instead of your waist or back.
- Control cough. Seek treatment for chronic cough or bronchitis, and don’t smoke.
- Avoid weight gain. Talk to your doctor to determine your ideal weight and get advice on weight-loss strategies if you need them.
Diagnosis
Posterior vaginal prolapse is usually diagnosed during a pelvic exam of the vagina and rectum.
During your pelvic exam, your doctor will likely ask for the following:
- That you bend down as if you were going to evacuate the intestines. Bending over can cause the posterior vaginal prolapse to protrude so that your doctor can assess its size and location.
- That you tense your pelvic muscles as if you were going to stop a flow of urine. This test is used to assess the strength of the pelvic muscles.
You may fill out a form that will help your doctor assess how far the lump extends into your vagina and how much it affects your quality of life. This information helps guide treatment decisions.
In rare cases, your doctor might also recommend imaging tests:
- Using an MRI or X-ray, the size of the protruding tissue can be determined.
- With a defecography, it can be determined how effectively the rectum empties.
Treatment
Treatment options depend on the severity of the posterior vaginal prolapse. Your doctor might recommend:
- Observation. If your posterior vaginal prolapse causes few or no symptoms, simple self-care measures, such as practicing Kegel exercises to strengthen your pelvic muscles, may provide relief.
- Pessary. A vaginal pessary is a plastic or rubber ring that is inserted into the vagina to support weakened tissues. The pessary should be removed regularly for cleaning.
Surgery
In the following cases, surgical repair may be required:
- If the posterior vaginal prolapse protrudes outside the vagina and is especially bothersome.
- If you suffer from prolapse of other pelvic organs, in addition to posterior vaginal prolapse, which causes discomfort. Surgical repair of each condition can be performed simultaneously.
Surgery usually involves removing the extra tissue that was stretched and causing the vaginal bulge, and placing stitches (sutures) to support the pelvic structure. A mesh patch may be inserted to support and strengthen the fascia.
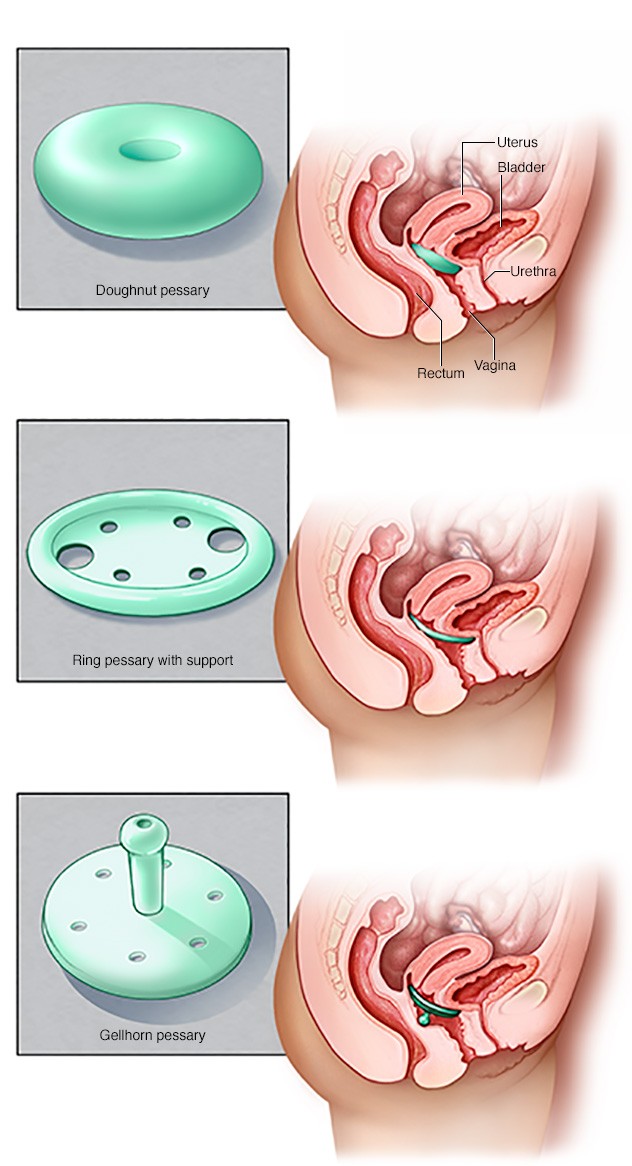
Pessaries come in many sizes and shapes. The device is placed in the vagina and works as a support for the vaginal tissues that are displaced by the prolapse of the pelvic organs. Your doctor can measure you for a pessary and help you decide which type of pessary is best for you.
Lifestyle and home remedies
Depending on the severity of the posterior vaginal prolapse, self-care measures may provide some relief. You could try:
- Perform Kegel exercises to strengthen your pelvic muscles and support weakened fascia.
- Avoid constipation by eating high-fiber foods and plenty of fluids.
- Avoid straining to have a bowel movement.
- Avoid heavy lifting.
- Control cough.
- Lose weight if you are overweight or obese.
Kegel exercises
Kegel exercises strengthen the pelvic floor muscles. A strong pelvic floor provides better support for the pelvic organs, prevents the prolapse from getting worse, and relieves symptoms associated with posterior vaginal prolapse.
To perform Kegel exercises:
- Squeeze (contract) your pelvic floor muscles as if you’re trying not to pass gas.
- Hold the contraction for five seconds, then relax for 10 seconds. If this is too difficult, start by holding for two seconds and relaxing for five seconds.
- Continue the exercise until you hold the contractions for 10 seconds at a time.
- Try to do at least three sets of 10 repetitions per day.
Kegel exercises may work best if taught by a physical therapist and reinforced with biofeedback. Biofeedback involves the use of control devices that help ensure that you are contracting your muscles properly for the optimal amount of time.
Once you’ve learned the proper method, you can do Kegel exercises discreetly at any time, whether you’re sitting at your desk or relaxing in an easy chair.
Preparation before the appointment
You may be referred to a gynecologist.
The following information will help you prepare for your appointment.
What can you do
- Make a list of the symptoms you have and indicate how long you have had them.
- Write down all medications, vitamins, and supplements you take, including dosages.
- Write down important personal and medical information, including other conditions, recent life changes, and stressors.
- Prepare questions to ask your doctor.
For posterior vaginal prolapse, some basic questions to ask your doctor include:
- What can I do at home to relieve symptoms?
- Should I limit any activity?
- What are the chances that the lump will get bigger if I do nothing?
- What treatment approach do you recommend?
- What is the chance that the posterior vaginal prolapse will come back if it is treated surgically?
- What are the risks of the surgeon?
During your consultation, feel free to ask other questions as they occur to you.
What to expect from the health professional
Your doctor will likely ask you a number of questions, such as:
- What symptoms do you have?
- When did you first notice symptoms? Have they gotten worse over time?
- Do you have pelvic pain?
- Do you have urine leaks?
- Have you had a severe or chronic cough?
- Do you lift heavy things in your work or daily activities?
- Do you force when evacuating the intestines?
- Has anyone in your family ever had posterior vaginal prolapse or other pelvic problems?
- How many children have you given birth to? Were your deliveries vaginal?
- Do you plan to have children in the future?