Polycystic ovary syndrome (PCOS) is a clinical syndrome characterized by moderate obesity, irregular periods or amenorrhea, and signs of androgen excess (eg, hirsutism, acne). Most patients have multiple ovarian cysts. Diagnosis is based on pregnancy test results, hormone measurements, and imaging to rule out a virilizing tumor. Treatment is symptomatic.
Polycystic ovary syndrome (PCOS) occurs in 5–10% of women. It is the most common cause of infertility in the United States.
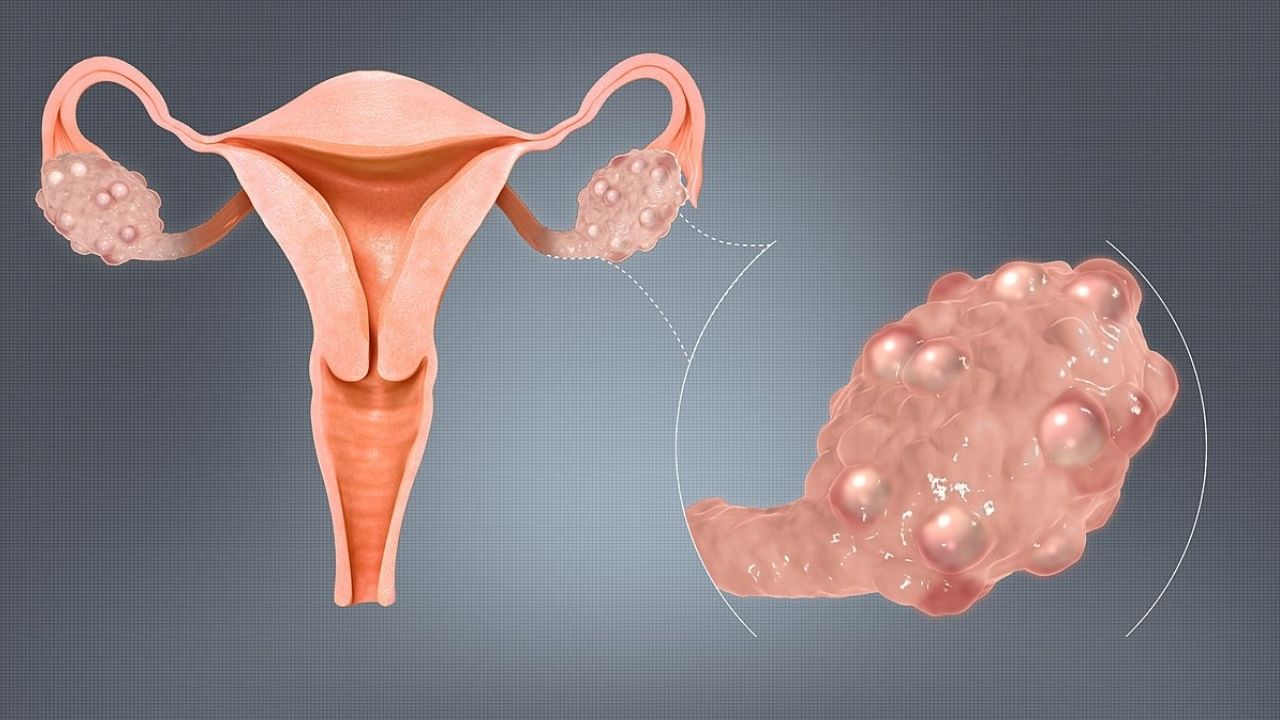
PCOS is usually defined as a clinical syndrome, regardless of cystic ovarian changes. But the presence in the ovary of many 2–6 mm or large follicular cysts containing atretic cells is typical. The ovaries can be normal in size or enlarged and have a thickened and smoothed tunica albuginea.
The syndrome is manifested by anovulation or ovulatory dysfunction and an excess of androgens of unknown etiology. However, there is some evidence that patients have a cytochrome P450c17 change that damages 17-hydroxylase (an enzyme that limits androgen production), resulting in increased androgen production.
Complications of polycystic ovary syndrome
Polycystic ovary syndrome has several serious complications.
Estrogen levels are elevated, which increases the risk of endometrial hyperplasia and ultimately endometrial cancer.
Androgen levels are often elevated, which increases the risk of metabolic syndrome and causes hirsutism. The possible presence of hyperinsulinemia due to insulin resistance may increase the production of androgens by the ovaries. Prolonged hyperandrogenism increases the risk of cardiovascular disease, including hypertension and hyperlipidemia.
The risk of increased androgen levels and related complications may be as high in women who are not overweight as in those who are.
Coronary artery calcification and carotid intimal thickening are more common in women with PCOS, suggesting possible subclinical atherosclerosis.
Also among these women, type 2 diabetes mellitus and impaired glucose tolerance are more common, and the risk of developing obstructive sleep apnea increases.
Recent research suggests that PCOS is associated with mild chronic inflammation and that women with PCOS are at increased risk of developing non-alcoholic fatty liver disease.
Symptoms of polycystic ovary syndrome
Symptoms of polycystic ovary syndrome usually appear during puberty and increase over time. Premature adrenarche characterized by excess dehydroepiandrosterone sulfate (DHEAS), often early axillary hair, body odor, and micromedonal acne are common.
Typical symptoms include mild obesity, mild hirsutism, and irregular menstruation, oligomenorrhea, or amenorrhea. However, about half of women with PCOS are of normal weight and some women are underweight. Body hair may be masculine (eg, on the upper lip, chin, back, thumbs and toes; around the nipples and along the white line below the abdomen). Some women have other signs of virilization, such as acne and temporary hair thinning.
Other symptoms may include weight gain (sometimes seemingly difficult to control), fatigue, lack of energy, sleep problems (including sleep apnea), mood swings, depression, anxiety, and headaches. Some women have impaired fertility. Symptoms vary from woman to woman.
Areas of hardened and darkened skin (acanthosis nigricans) may appear in the armpits, the nape of the neck, skin folds, and in the finger and / or elbow folds; the cause is high insulin levels due to insulin resistance.

If women with PCOS become pregnant, the risk of pregnancy complications increases, and these complications are usually more severe if women are obese. These complications include gestational diabetes mellitus, preterm labor, and preeclampsia.
Tests for polycystic ovary syndrome
- Clinical criteria
- Serum levels of testosterone , follicle stimulating hormone (FSH), prolactin, and thyroid stimulating hormone (TSH)
- Ultrasound of the pelvic organs
Ovulatory dysfunction usually occurs during puberty, resulting in primary amenorrhea; thus, polycystic ovary syndrome is unlikely in cases where regular menses have been observed for some time after menarche.
Patients with polycystic ovary syndrome (PCOS) usually have profuse cervical mucus on examination, reflecting high estrogen levels. PCOS should be suspected if a woman has two typical symptoms.
The examination includes a pregnancy test, blood levels of total testosterone, prolactin and TSH; ultrasound examination of the pelvic organs to rule out other possible causes of existing symptoms. Serum free testosterone testing is more sensitive than total testosterone testing, but technically more difficult to measure. Normal or slightly elevated testosterone levels and normal or slightly elevated FSH levels suggest PCOS.
To make a diagnosis, at least 2 of the 3 criteria below must be met:
- Ovulatory dysfunction causing irregular periods
- Clinically and laboratory proven hyperandrogenism
- More than 10 follicles in each ovary (detected by ultrasound of the pelvic cavity), usually located in the periphery and resembling a string of pearls
In women with these criteria, the serum cortisol level is measured to exclude Cushing’s syndrome, and the early morning level of 17-hydroxyprogesterone is measured to exclude adrenal virilization. Serum DHEAS is measured. If the DHEAS level is not normal, the woman is examined in the same way as for amenorrhea .
A transvaginal ultrasound can be used to check for abnormalities in the ovaries. However, transvaginal ultrasound is not done in adolescent girls.
Common Sense and Caveats
The diagnosis of polycystic ovary syndrome is unlikely if menstruation has been regular for some time after menarche.Testosterone levels are measured in adolescents with PCOS symptoms.
Diagnosing PCOS in adolescent girls
Diagnosing PCOS in adolescents is difficult because physiological changes during puberty (eg, hyperandrogenism, menstrual irregularities) are similar to those of PCOS. Thus, separate criteria were proposed for the diagnosis of PCOS in adolescents: however, no consensus was reached. These criteria require the following two conditions:
- Abnormal uterine bleeding (abnormal for age or gynecologic age, or symptoms that persist for 1–2 years)
- Signs of hyperandrogenism (based on persistent increases in testosterone levels above the adult norm [best evidence], moderate to severe hirsutism, or moderate to severe inflamed acne vulgaris, as an indication for a hyperandrogenism test)
Often, a 17-hydroxyprogesterone test is also done to detect nonclassical congenital adrenal hyperplasia.
Pelvic ultrasound is usually only indicated if serum androgen levels or virilization indicate the presence of an ovarian tumor. Transvaginal ultrasonography is not commonly used to diagnose PCOS in adolescent girls because it detects polycystic morphology in <40% of girls and by itself does not predict the presence or development of PCOS.
Treatment for polycystic ovary syndrome
- Intermittent courses of progestins or oral contraceptives
- Treatment of hirsutism, and in adult women – the risk of long-term hormonal disorders
- Fertility treatment for women wishing to become pregnant
The goal of treatment for polycystic ovary syndrome is
- Correction of hormonal disorders and thereby reducing the risks associated with excess estrogen (for example, endometrial hyperplasia) and excess androgens (for example, cardiovascular disease)
- Relief of symptoms and improvement of fertility
Weight loss and regular exercise are recommended. They can promote the induction of ovulation, increase the regularity of the menstrual cycle, increase sensitivity to insulin sensitivity, and reduce the appearance of acanthosis nigricans and hirsutism. Losing weight can also help improve fertility. However, weight loss is unlikely to benefit normal-weight women with PCOS.
Hormonal contraceptives are the first line therapy for menstrual irregularities, hirsutism and acne in women with PCOS and those who do not wish to become pregnant. To reduce the risk of hyperplasia and endometrial cancer, women are usually given intermittent courses of progestins (eg, oral medroxyprogesterone acetate, 5–10 mg once daily for 10–14 days every 1–2 months) or combined oral contraceptives. This treatment results in a decrease in circulating androgen levels and tends to help shape a more regular menstrual cycle.
Metformin 500 to 1000 mg 2 times a day is used to increase the level of sensitivity to. When using metformin, it is necessary to measure the level of glucose in the blood serum, as well as to carry out periodic tests of the function of the kidneys and liver. Since metformin can induce ovulation, contraception is needed if pregnancy is not desired. Metformin helps correct metabolic and glycemic abnormalities and makes menstrual cycles more regular, but has little or no positive effect on hirsutism, acne, or infertility. insulin sensitivity in women with PCOS, irregular menstruation and diabetes or insulin resistance if lifestyle changes are ineffective or if they cannot or cannot tolerate hormonal contraceptives. Metformin can also lower free testosterone levels
Women wishing to become pregnant should be referred to a fertility specialist. Drugs used for the treatment of infertility (e.g., clomiphene). Clomiphene is currently the first line of treatment for infertility. Weight loss is also beneficial. Hormone therapy, which may have a contraceptive effect, is avoided. Letrozole, an aromatase inhibitor, can also stimulate ovulation. You can also try other fertility drugs. These include follicle- stimulating hormone (FSH) to stimulate the ovaries, a gonadotropin-releasing hormone (GnRH) agonist to stimulate the release of FSH, and human chorionic gonadotropin (hCG) to stimulate ovulation.
Because women with PCOS have a higher risk of pregnancy complications (including gestational diabetes mellitus, preterm labor, and preeclampsia) that are exacerbated by obesity, a preliminary body mass index, blood pressure measurement, and oral glucose tolerance test are recommended. If clomiphene and other drugs are ineffective or if there are other indications for laparoscopy, laparoscopic ovarian drilling may be considered; however, possible long-term complications of drilling (eg adhesions, ovarian failure) should be considered. Ovarian drilling involves using an electrocautery or laser to drill holes in small areas of the ovaries that produce androgens. Ovarian resection is not recommended.
With hirsutism physical measures can be used (eg, bleaching, electrolysis, plucking, waxing, epilation). To remove unwanted facial hair, twice daily use of 13.9% eflornithine cream (not registered in the Russian Federation) can help. In adult women who do not want to become pregnant, hormone therapy can be used to lower androgen or spironolactone levels. Spironolactone 50–100 mg twice daily is effective, but since this drug can be teratogenic, effective contraception is required. Cyproterone, an antiandrogen (not available in the US), reduces unwanted body hair in 50–75% of women with such problems. Weight loss reduces androgen production in obese women and thus can slow hair growth.
GnRH agonists and antagonists are being studied as treatments for unwanted body hair. Both groups of drugs suppress the production of sex hormones by the ovaries. However, both can cause bone loss and lead to osteoporosis.
PCOS Acne can be treated with conventional medications (benzoyl peroxide, tretinoin cream, topical and general antibiotics). Systemic isotretinoin is used only in severe cases.
Control of comorbidities
Because PCOS increases the risk of depression and anxiety, women and adolescents with PCOS should be evaluated for these problems based on their history and, if a problem is identified, they should be referred to a mental health professional and / or treated as needed.
Overweight or obese adolescents and women with PCOS should be screened for symptoms of obstructive sleep apnea using polysomnography and treated as needed.
Because PCOS can increase the risk of cardiovascular disease, referral to a cardiologist for prevention of cardiovascular disease is necessary if women with PCOS have any of the following risk factors:
- Family history of early cardiovascular disorders
- Smoking
- Diabetes
- Arterial hypertension
- Dyslipidemia
- Sleep apnea
- Abdominal obesity (like metabolic syndrome )
Clinicians should assess the risk of cardiovascular disease by determining body mass index (BMI), measuring fasting lipid and lipoprotein levels, and identifying risk factors for metabolic syndrome.
Adult women with PCOS are screened for metabolic syndrome by measuring blood pressure and serum glucose and lipids (lipid profile).
To detect subclinical atherosclerosis, tests should be done for coronary artery calcification and intimal thickening of the middle carotid artery.
Women with abnormal vaginal bleeding should be screened for endometrial carcinoma using endometrial biopsy and / or transvaginal ultrasound or office hysteroscopy.
Outlook
- Polycystic ovary syndrome (PCOS) is a common cause of ovulatory dysfunction.
- PCOS should be suspected in women with irregular periods, mild obesity, and mild hirsutism, but it should also be remembered that many women with PCOS may be of normal or reduced weight.
- Screening should be done for serious conditions (eg, Cushing’s syndrome, tumors) that have similar symptoms, and for complications (eg, metabolic syndrome)
- If pregnancy is undesirable, it is necessary to treat women with hormonal contraceptives and recommend lifestyle changes; if lifestyle changes are ineffective, metformin should be added.
- If women with PCOS are infertile and wish to become pregnant, they should be referred to a fertility specialist.
- Screening for comorbid conditions such as endometrial cancer, mood and anxiety disorders, obstructive sleep apnea syndrome, diabetes, and cardiovascular risk factors (including hypertension and hyperlipidemia) is needed.