What is vasculitis?
Vasculitis (plural: vasculitides) is a generic term for different forms of vascular inflammation. Vasculitis often causes pain in joints or muscles, and occasionally joint swelling. Therefore, they are considered rheumatic diseases. A distinction is made between primary vasculitis and secondary vasculitis.
There is no known underlying disease in primary vasculitis. Secondary vasculitis is when the vascular inflammation occurs in connection with another disease or after taking medication.
Vasculitis is rare. Estimates show that around 200,000 people in Germany suffer from vasculitis or collagenosis. Depending on which blood vessels (large or small blood vessels) are affected, very different clinical pictures develop.
Causes of vasculitis
The vascular inflammation is caused by a faulty immune reaction. The immune system mistakenly sees the body’s own substances as foreign and fights them. As a result, the wall of the blood vessel becomes inflamed and swollen. The vessel lumen becomes narrower.
Organs can no longer be adequately supplied with blood and no longer work properly. Why this process occurs is not yet known. Scientists suspect that genetic causes and environmental influences promote the development of the disease.
Symptoms of vasculitis

In most cases, vasculitis does not break out suddenly, but rather slowly announces itself. Because the organs do not receive enough nutrients, the disease initially makes itself felt like a completely normal infection.
Signs of vasculitis can include:
- Musculoskeletal complaints (muscle and joint pain, rarely swelling of the joints)
- Eye redness
- Visual disturbances
- A headache
- Ear, nose and throat problems (bloody runny nose or sudden hearing loss)
- Numbness (e.g. of the feet)
- Discomfort in the gastrointestinal tract (bloody diarrhea, abdominal pain)
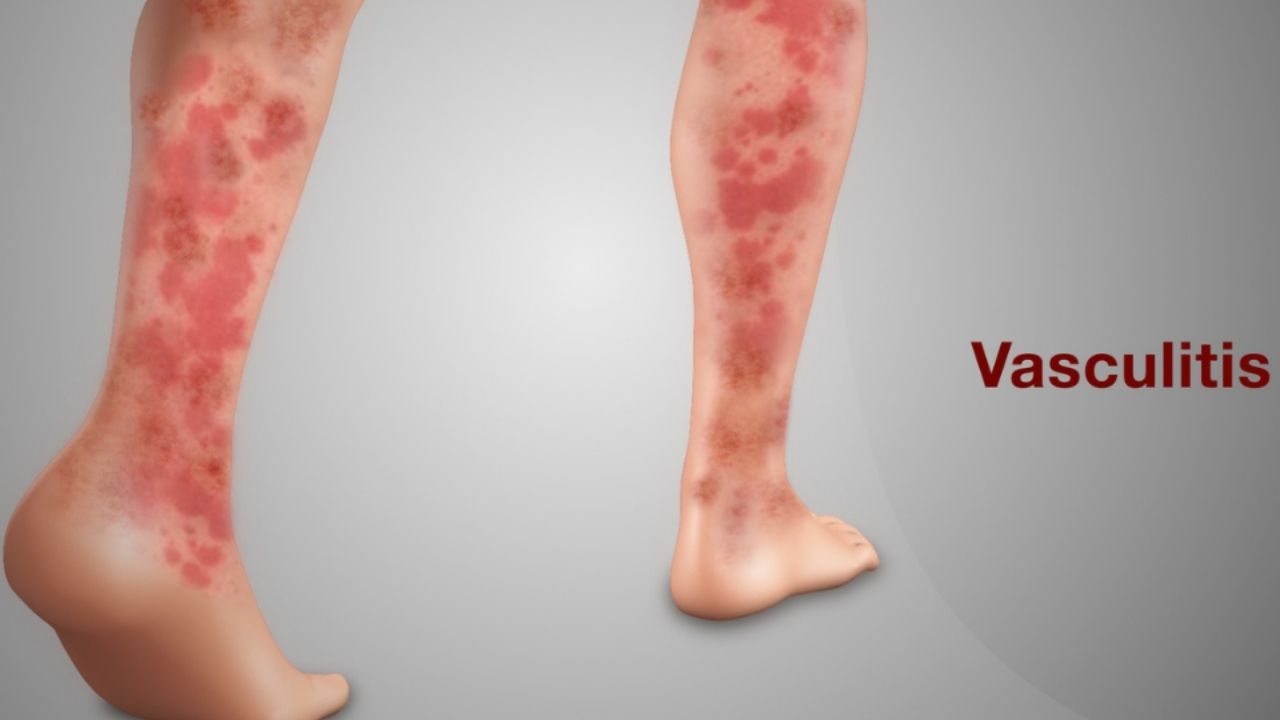
- Skin changes (red spots, nodules, ulcers)
- Coughing up blood
- Bloody urine
The first general symptoms can be:
- fatigue
- Weight loss
- fever
- Body aches
- Night sweats
Many of the symptoms can also have other causes. However, the doctor should be alerted if several of the signs appear in different organs.
Diagnosis of vasculitis
If vasculitis is suspected, the diagnosis begins with a questioning of the person concerned (anamnesis) and a physical examination. If the symptoms have already appeared in the past, this can be an important indication. If the initial suspicion solidifies, the next steps follow.
Laboratory tests
Doctors can use laboratory tests to determine whether there is inflammation in the body. The erythrocyte sedimentation rate (ESR) is accelerated and the value of a certain protein (C-reactive protein) is increased.
However, the examinations say nothing about the type of inflammation. If so-called auto-antibodies can be found in the blood, this is also an important indication.
Antibodies are proteins that the body produces to fight off foreign bodies. Auto-antibodies also attack your own body. Their existence suggests auto-immune disease.
The type of auto-antibodies indicates which auto-immune disease is involved. ANCA (= anti-neutrophil cytoplasmic antibodies) are typical of vasculitis. However: if auto-antibodies are missing, this does not rule out vasculitis.
A urine analysis can also provide important information – especially about whether the disease has affected the kidneys.
Imaging procedures
With the aid of imaging procedures, the doctor can find out where something has changed in the body. This is important for the diagnosis, but also for deciding where a tissue sample makes sense. Imaging tests also help assess whether a therapy will work.
With the help of sonography, magnetic resonance and computed tomography, the doctor can determine changes in the head and internal organs. An x-ray can show whether the disease has infected the lungs.
Biopsy
A tissue examination (biopsy) can provide information about whether there are inflammatory changes in the blood vessels. To do this, the doctor takes a tissue sample – for example from the nose, lungs, kidney or from a branch of the temporal artery.
Treatment for vasculitis – what are the options?
There is no cure for vasculitis, but it can be treated well today. The therapy for vasculitis depends on which vessels and organs are affected and how far the disease has progressed.
Medicinal treatment
Medicinal treatment Cortisone almost always plays an important role in the treatment of vasculitis . It quickly inhibits inflammation and slows the immune system attacking its own body. However, cortisone can have side effects, including:
- Weight gain
- Skin changes
- Lens opacity
- Increased intraocular pressure
- high blood pressure
- osteoporosis
- diabetes
- Infectious tendency
These side effects can be reduced if patients follow certain rules when taking it (therapy rules for cortisone). This includes:
- A calcium-rich diet
- Vitamin D supplements
- Regular check-ups at the ophthalmologist
With some forms of vasculitis, treatment with cortisone is sufficient (mostly with giant cell arteritis, Schönlein Hennoch purpura), with other forms additional agents that inhibit the immune system are required.
The drug cyclophoshamide is very effective, but also extremely aggressive. It is therefore only used when the situation is life-threatening – and then only for as short as possible.
If the kidneys are also heavily involved, blood washing (plasmapheresis) can relieve the organs. If the disease is less severe, the active ingredient methotrexate can be sufficient and help to save on cortisone.
As soon as the inflammation has subsided, treatment can be switched to better tolerated agents, such as azathioprine or cotrimoxazole.
To avoid relapse, patients usually have to take these drugs for years, often also a small dose of cortisone. Standard drugs do not work in some patients with life-threatening vasculitis.
Doctors can then switch to other therapies, for example biologics, active ingredients manufactured using biotechnology. One of these agents is rituximab. It blocks the cells that attack your own body.
Another alternative is the drug mycophenolate mofetil (MMF), which suppresses the effect of the immune system.
Non-drug treatment
All vasculitis drugs have side effects. But there is no alternative to them. Patients who forego conventional medical treatment risk their lives. It is therefore always important that patients consult their doctor before starting any complementary therapy. Given the rarity of vasculitides, patient training is also particularly important.
Diet
In general, it is advisable for people with a chronic inflammatory disease to eat a low-meat diet. That means: a maximum of two small portions of meat per week. Arachidonic acid is found in meat. It promotes inflammation. A low-meat diet has anti-inflammatory effects.
If you consume enough omega-3 fatty acids, this effect can be increased. Two servings of high-fat fish per week is enough to reduce the risk of inflammation. Alternatively, if you don’t like fish, you can take fish oil capsules.
Vitamins E and C also have anti-inflammatory effects. Vitamin C is found in fresh fruits and vegetables. Besides meat, vitamin E is mainly found in certain vegetable oils. Nutritional therapy alone is never enough.
It can support and complement the basic therapy. In individual cases, therapy may make it possible to take anti-inflammatory drugs in a lower dose. But good nutrition can never replace drug therapy.
Movement
also movement facilitates the handling of the disease. Physiotherapy and functional training keep sore joints and muscles flexible. Movement is also important for inner balance.
Relaxation excercise
Relaxation exercises can also contribute to a balanced basic posture. They can also reduce pain. Effective relaxation methods are, for example, autogenic training or progressive muscle relaxation according to Jacobson.
Psychological support
A chronic disease like vasculitis not only stresses the body, but also the psyche. The constant exhaustion, the drop in performance and the fear of the future cause problems for many patients.
In addition, the drugs often have a negative effect on mood. In these cases a psychologist can help. Talking to an outsider about these issues is often easier than talking to friends or loved ones.
In addition, the professional view makes it easier to deal with the problems. And psychologists don’t just show the patient understanding. They also know how to solve the problems.
It is important to clarify before the treatment whether the health insurance will cover the costs for the psychological therapy.
Operation
In rare cases, larger vessels can be stretched with a stent (tube) if they are blocked as a result of vasculitis.