In an ectopic pregnancy, the fertilized egg implants in the fallopian tube rather than in the uterus. This can happen if the fallopian tube is not completely drained. The fallopian tube can rupture as the embryo grows. The result is life-threatening bleeding in the abdominal cavity. Since the symptoms of an ectopic pregnancy hardly differ from those of a normal pregnancy, only a specialist doctor can make the diagnosis. Read more about ectopic pregnancy here!
Quick overview
• What is an ectopic pregnancy? Pregnancy in which the fertilized egg implants in the fallopian tube instead of the uterus. Most common form of ectopic pregnancy (pregnancy with implantation of the embryo outside the uterus).
• Causes: Fallopian tubes that are not or not completely permeable. Various risk factors such as blocked or kinked fallopian tubes, polyps, previous tubal infections, previous tubal pregnancies, abdominal or pelvic surgeries, smoking, IUDs, fertility disorders, artificial insemination, etc.
• Ectopic pregnancy symptoms: labor-like abdominal pain, vaginal bleeding, dizziness, circulatory problems, general malaise.
• Complication: ruptured fallopian tube with severe bleeding into the abdominal cavity and circulatory shock (danger to life!).
• Treatment: Depends on the stage of ectopic pregnancy. Usually surgical removal of the embryo, if possible with preservation of the affected fallopian tube. In a very early stage possibly drug treatment. Sometimes waiting under medical supervision (the embyro can spontaneously pass by itself).
• Prognosis: Complete recovery with proper treatment. Subsequent pregnancies can be completely normal.
Description of ectopic pregnancy
At around 96 percent, tubal pregnancy is the most common form of so-called extrauterine pregnancy (EUG). This refers to pregnancies in which the fertilized egg implants itself outside the uterus (ectopic implantation). In the case of ectopic pregnancy, the ovum gets lodged in the fallopian tube. In other types of extrauterine pregnancy, the egg implants itself in the ovaries (ovarian pregnancy), in the cervix (cervical pregnancy), or in the abdominal cavity (peritoneal pregnancy). It cannot be discharged.
Ectopic pregnancy accounts for one to two percent of all pregnancies.
Types of ectopic pregnancy
Doctors differentiate between three types of tubal pregnancy, depending on where in the fallopian tube the egg implants itself:
• Ampullar tubal pregnancy: Implantation takes place in the first third of the fallopian tube.
• Isthmic ectopic pregnancy: The fertilized egg implants itself in the last third of the fallopian tube, just before it opens into the uterus.
• Interstitial/intramural pregnancy: The fertilized egg implants itself at the transition from the fallopian tube to the uterus.
An ectopic pregnancy cannot be carried to term. Without treatment, the growing embryo can rupture the fallopian tube. This causes life-threatening bleeding in the abdominal cavity.
Causes of ectopic pregnancy
Normally, the fertilized egg travels down the fallopian tube into the uterus and implants there. However, if the fallopian tube is not permeable or only partially permeable, the egg gets stuck in it on its way into the uterus and grows firmly. The patency of a fallopian tube can be impaired for various reasons. These include:
- Adhesion or kinking of the fallopian tube.
- Tubal polyps.
- Congenital anatomical features such as cavities in the wall of the fallopian tube.
- Scars or adhesions of the ovaries, for example due to previous operations in the abdominal or pelvic area.
- Previous fallopian tube infections, especially if caused by chlamydia.
- Previous ectopic pregnancies.
- Fertility disorders and artificial insemination.
- Local damage to the fallopian tubes, for example due to endometriosis (foci of scattered uterine lining, for example in the fallopian tubes).
- Abortions.
- Miscarriages.
- Muscle weakness.
- Too few cilia on the inner wall of the fallopian tubes (the hair-thin cilia drive the egg cell forward in the fallopian tube).
- Hormonal imbalance.
- Tuberculosis.
Smoking also promotes the development of an ectopic pregnancy. Nicotine restricts the mobility of the cilia.
Women who use a spiral for contraception also have an increased risk: the spiral makes it easier for microorganisms to access the fallopian tubes, where they can cause inflammation. These in turn favor an ectopic pregnancy.
The number of ectopic pregnancies has increased in recent decades. Experts discuss various reasons for this, including increased fallopian tube inflammation due to sexually transmitted diseases, more frequent fertility treatments, use of IUDs as contraceptives and smoking.
Ectopic pregnancy symptoms
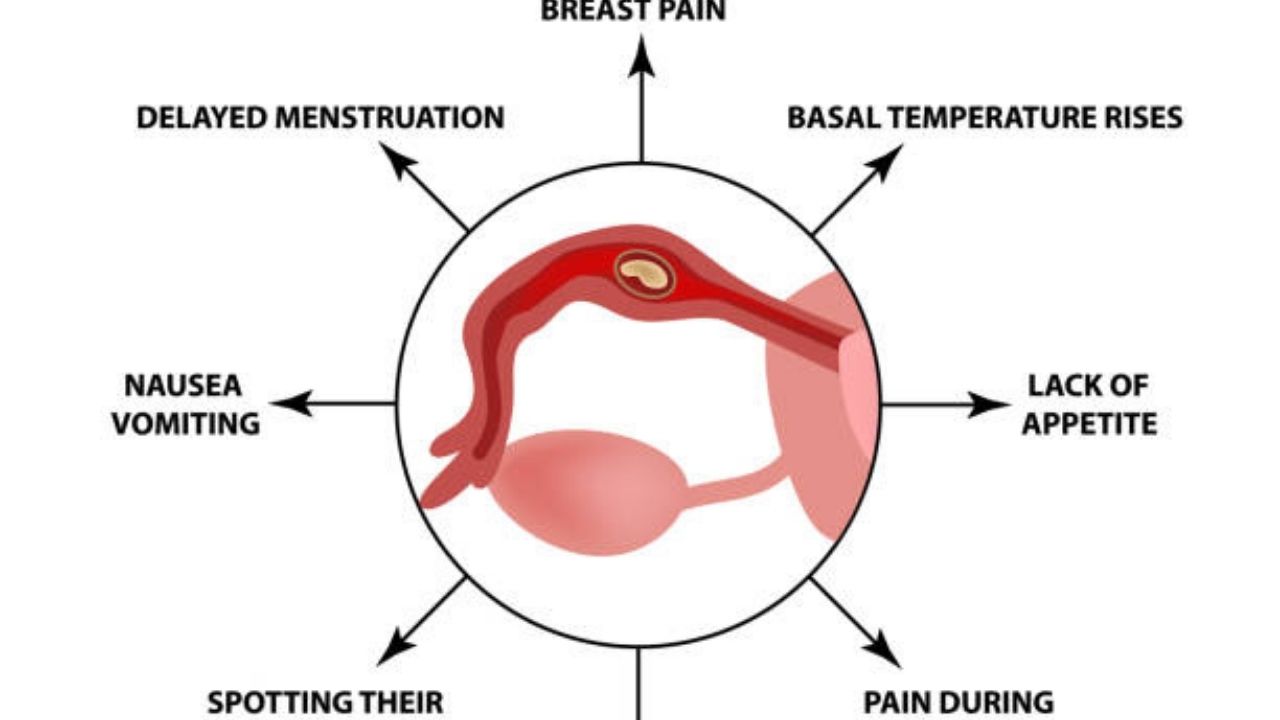
An ectopic pregnancy initially proceeds like a normal pregnancy:
- Missed period.
- Morning sickness (may also occur at other times of the day).
- Feeling of tension in the breasts.
Even a pregnancy test cannot distinguish between a normal and an ectopic pregnancy. It also shows a positive result for the latter. Because the placenta forms the pregnancy hormone beta-HCG (human chorionic gonadotropin) in an ectopic pregnancy as in a normal pregnancy, to which the test reacts positively.
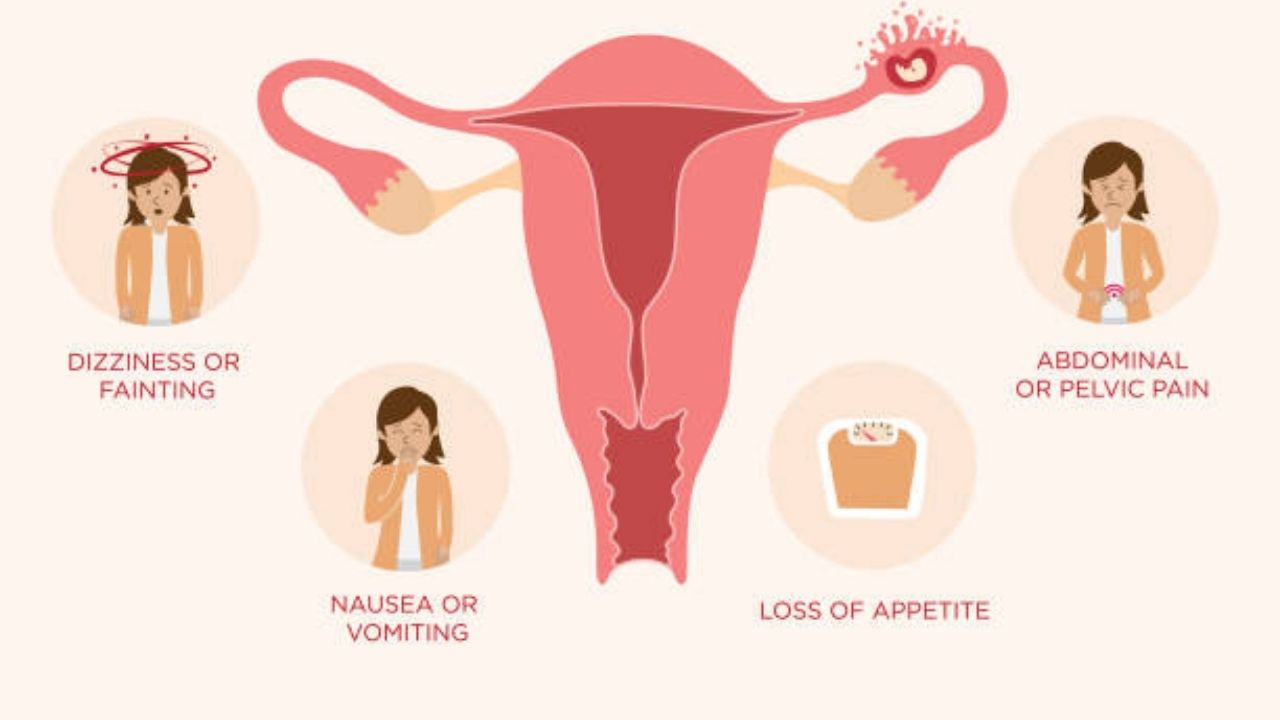
Ectopic pregnancy signs
The signs of an ectopic pregnancy typically do not appear until between the sixth and ninth week of pregnancy. These include:
- Unusual, usually unilateral, cramping or labor-like abdominal pain.
- Tense abdominal wall that reacts sensitively to touch.
- Bleeding from the vagina (often as a faint brownish discharge = spotting, but sometimes also dark red with clots of clotted blood and/or tissue parts).
- Dizziness and paleness.
- Shortness of breath.
- Fast pulse.
- Nausea and vomiting.
- General malaise.
- Slightly elevated temperature.
The symptoms of an ectopic pregnancy can vary from woman to woman. They can also appear suddenly and intensely or slowly increase.
The symptoms mentioned are not specific to an ectopic pregnancy. Similar symptoms can also occur with inflammation of the renal pelvis, appendicitis, ovarian inflammation or fallopian tube inflammation. Only a doctor can determine the exact cause of the symptoms.
Complications of ectopic pregnancy
About three out of ten women with an ectopic pregnancy develop complications: The fallopian tube ruptures due to the growing embryo. Important blood vessels (usually the uterine artery or the ovarian artery) are injured. The consequences are severe internal bleeding. Warning signs of this are suddenly onset, very severe, one-sided abdominal pain that can radiate to the upper abdomen, back and shoulders. The loss of blood can cause dizziness, fainting or circulatory shock.
If you have any signs of an ectopic pregnancy, you should consult a doctor immediately. If the fallopian tube ruptures, there is a risk of death! Then alert the emergency doctor immediately!
Ectopic pregnancy
Like an ectopic pregnancy, a very rare ectopic pregnancy is a form of extrauterine pregnancy: the fertilized egg falls through the upper opening of the fallopian tube into the abdominal cavity and nests here – usually on the intestinal wall or the back wall of the uterus.
An abdominal cavity pregnancy is usually discovered during preventive ultrasound examinations. The embryo in the abdominal cavity is usually not viable. In most cases, it will die off on its own. If that doesn’t happen, it’s surgically removed.
Diagnosis of ectopic pregnancy
If an ectopic pregnancy is suspected, the gynaecologist will first discuss the patient’s medical history: He will have the symptoms described in detail and will inquire about any risk factors (previous ectopic pregnancies, tubal inflammation, miscarriage or abdominal surgery, endometriosis, etc.).
Gynecological check
This is followed by a vaginal palpation: the internal and external palpation is part of the normal gynecological examination. The doctor can gain important information from this. In the case of an ectopic pregnancy, the uterus is smaller than it actually should be based on the current week of pregnancy. The doctor may also notice during the palpation that a fallopian tube is enlarged on one side.
Feeling the fallopian tube where the embryo has implanted can be a bit painful.
Ultrasound
Where exactly a fertilized egg cell has implanted can usually be determined by means of an ultrasound examination. It can be done through the vagina (transvaginal sonography). This makes it possible to determine whether the pregnancy is normal (i.e. with implantation in the uterine cavity). If no egg is visible in the uterus, this can be due to the following reasons:
• The embryo has implanted itself in the uterus, but it is still too small to be detected by ultrasound. The pregnancy is then less advanced than you would have thought based on the last observed menstrual period.
• Although the embryo was in the uterus, it was rejected (miscarriage, abortion).
• The embryo has actually implanted itself outside the uterus (extrauterine pregnancy such as ectopic pregnancy).
To check the third option, the gynecologist can use a special variant of the ultrasound examination, color Doppler sonography. It can make tissue that is particularly well supplied with blood visible – for example the mucous membrane area in which the egg cell has implanted itself (e.g. in the fallopian tube).
Blood test
In addition, the doctor can determine the amount of the pregnancy hormone beta-HCG (human chorionic gonadotropin) in the blood of the pregnant woman several times over a long period of time. In normal pregnancies, blood levels of this hormone double every two days. If, on the other hand, the egg implanted itself incorrectly (as in the case of an ectopic pregnancy), the HCG level rises only slowly, stagnates or even falls again.
Laparoscopy
In unclear cases, the doctor can also perform a laparoscopy . In this way, it can be determined with certainty whether an ectopic pregnancy is actually present. If so, the incorrectly implanted egg cell can also be removed during the examination (see: Treatment).
Treatment of ectopic pregnancy
Depending on how far the ectopic pregnancy has progressed, there are different treatment approaches.
Laparoscopy
If an ectopic pregnancy is associated with abdominal pain, the onset of bleeding in the abdominal cavity, or abnormal HCG levels, a laparoscopy is usually necessary. This allows the ectopic pregnancy to be recognized and treated at the same time. During the procedure, the doctor inserts an endoscope into the abdominal cavity through three small incisions in the abdominal wall. This is a thin flexible tube with a light source and a small camera at the tip. The doctor can insert the finest medical instruments through the endoscope in order to remove the embryo from the fallopian tube.
Open operation
In some cases of ectopic pregnancy, open surgery (laparotomy) is necessary: the surgeon opens the abdominal wall with a larger incision to remove the embryo in the fallopian tube. An open operation is necessary, for example, if a laparoscopy is not possible for certain reasons, the woman has extensive adhesions or an unstable circulation. Even in cases where the ectopic pregnancy has already resulted in a ruptured fallopian tube, open surgery is required. This is the only way to stop the heavy bleeding as quickly as possible.
If the bleeding is very heavy or the fallopian tube is severely damaged, it sometimes has to be removed completely. However, doctors always try to preserve the fallopian tube if at all possible.
Medication
A very early ectopic pregnancy can also be treated with medication in individual cases. Methotrexate is usually administered to pregnant women. The attending doctor injects the cell toxin under ultrasound control into the amniotic sac, causing the embryo to die. In the days that follow, the doctor regularly checks whether the beta-HCG level in the pregnant woman’s blood is falling. This drop indicates that the pregnancy is actually terminated.
Drug treatment is only possible under certain conditions. The ectopic pregnancy must not yet cause any symptoms. In addition, the embryo, together with the surrounding tissue, must be less than four centimeters. Last but not least, the HCG level in the blood of the pregnant woman must be below a certain threshold.
Wait and watch
Many ectopic pregnancies end of their own accord within the first three months of pregnancy. Since the fallopian tube does not offer enough space for the growing embryo and cannot guarantee its adequate supply, the egg cell ruptures. The placenta and amniotic sac then detach from the wall of the fallopian tube. They pass naturally with the embryo.
If there are no symptoms and at the same time the level of the pregnancy hormone beta-HCG in the blood is exceptionally low, you can possibly wait a few days before starting therapy. The pregnant woman is carefully monitored. If the concentration of the pregnancy hormone continues to fall during this time and the embryo stops growing, the pregnancy is very likely to be over. However, if the embryo continues to grow, the fallopian tube can rupture within a very short time and lead to dangerous bleeding. You have to be prepared for this possibility: It must be ensured that in such an emergency the pregnant woman can be operated on quickly.
Ectopic pregnancy: course and prognosis
An ectopic pregnancy often goes unnoticed and ends by itself – the incorrectly implanted egg cell is rejected together with the placenta. If this does not happen, the ectopic pregnancy should be terminated as early as possible with surgery or medication.
Drug treatment is considered to be gentler on the affected fallopian tube than surgery, but is only possible in certain cases. If a surgical intervention (laparoscopy, open surgery) cannot be avoided, the fallopian tube can be preserved in most cases. Its patency is usually still 80 to 90 percent after the operation. The same applies, by the way, if the ectopic pregnancy is treated with medication.
on various factors. For example, it matters how badly the fallopian tube was damaged by the ectopic pregnancy, whether it needs to be removed, and how well the second fallopian tube is functioning. It also has an influence whether the woman has already had more than one extrauterine pregnancy. For example:
After a first ectopic pregnancy that was surgically terminated (while preserving the affected fallopian tube), the risk of a second such ectopic pregnancy is around 15 percent. If a woman has already had two ectopic pregnancies, the “risk of recurrence” is about 40 percent.
In general, however, more than half of all women who have had an ectopic pregnancy (or other extrauterine pregnancy) will have a child later.
Getting pregnant after an ectopic pregnancy
You may be wondering if it is possible to have a healthy pregnancy after an ectopic pregnancy. It is best to talk to your doctor so that he can guide you taking into account your medical history. If the affected fallopian tube is still intact, you have a good chance of having a healthy pregnancy in the future. Even if one of your tubes has been removed, there is still a chance that a sperm could fertilize an egg in the other tube and the fertilized egg could reach the uterus.
However, keep in mind that having an ectopic pregnancy increases the chances of it happening again the next time, so if you do get pregnant again, watch closely for signs and symptoms until your doctor confirms that the egg is in the right place, that is, the uterus.
Ectopic pregnancies are rare, but if you experience any symptoms that worry you, don’t hesitate to talk to your doctor for reassurance and advice.
Can a pregnancy test give me a positive if I have an ectopic pregnancy?
Many pregnancy tests are used to check for the presence of the hormone hCG, so they may be positive until treatment to terminate the ectopic pregnancy has been completed.
How can i know if I have an ectopic pregnancy?
Your doctor will be able to confirm this, but you may notice some symptoms such as abnormal vaginal bleeding, sharp pain in your pelvis, abdomen, or shoulders, or feeling dizzy or weak.
If I have an ectopic pregnancy, where will I feel pain?
The pain may appear in the abdomen, pelvis or shoulders. You may also feel generally unwell, feel weak, and have an upset stomach or tender breasts.
How far can an ectopic pregnancy progress?
Once the ectopic pregnancy is diagnosed, the doctor will recommend when to start treatment. If you have a ruptured fallopian tube, you will likely need emergency surgery.
