Hemolytic anemia occurs when red blood cells are destroyed or broken down too early. The causes are manifold. Typical symptoms are paleness, fatigue, yellowing of the skin and mucous membranes and an enlarged spleen. Read here how hemolytic anemia progresses and what doctors do about it!
ICD codes for this disease: D57 | D59 | D56 | D55 | D58
Overview:
- What is hemolytic anemia? Anemia due to destruction or premature breakdown of red blood cells (erythrocytes).
- Disease course and prognosis: Course and prognosis depend on the underlying cause.
- Symptoms: paleness, weakness, circulatory problems up to fainting, headache, abdominal pain, back pain, yellowing of the skin and mucous membranes (icterus), enlargement of the spleen (splenomegaly).
- Causes: Congenital or acquired diseases, medicines, drugs
- Diagnostics: Typical symptoms, blood test, blood smear, Coombs test, ultrasound, bone marrow biopsy.
- Treatment: glucocorticoids (cortisone), immunosuppressants (medicines that reduce the immune system), bone marrow transplantation, removal of the spleen, administration of folic acid and iron.
- Prevention: No specific precautionary measures are possible.
What is hemolytic anemia?
Hemolytic anemia is what doctors call anemia that is caused by the destruction or premature breakdown of red blood cells (erythrocytes). Normally, red blood cell breakdown and regeneration follow a cycle: Healthy erythrocytes have a life cycle of around 120 days (70 to 90 days in newborns) before they are broken down and regenerated in the bone marrow.
In the case of hemolytic anemia, this cycle is shortened: the red blood cells are broken down prematurely (after around 30 days on average), and new formation in the bone marrow lags behind. Overall, there are too few erythrocytes in the blood and breakdown products of the blood cells are deposited in the body. Typical signs of hemolytic anemia are paleness, tiredness, dizziness, circulatory problems, yellowing of the skin and an enlarged spleen.
Hemolytic anemia has many possible causes, some are congenital ( e.g., thalassemia, sickle cell anemia, globule cell anemia, favism), others are acquired over the course of life. Examples of acquired hemolytic anemias are autoimmune hemolytic anemia, rhesus intolerance, malaria, lead poisoning, incompatible blood transfusions, severely elevated copper levels and paroxysmal nocturnal hemoglobinuria.
In addition, doctors distinguish whether the cause of the hemolysis lies in the red blood cells themselves (corpuscular anemia) or outside of the blood cells (extracorpuscular anemia).
What is hemolysis?
Hemolysis is the dissolution of red blood cells. This destroys the covering (cell membrane) that surrounds the red blood cell. Hemolysis in itself is not a disease, it happens all the time in every body: red blood cells have a life cycle of about 120 days. After that, they are dismantled and replaced with new ones. The bone marrow is responsible for the new formation of red blood cells: This is where new erythrocytes develop from progenitor cells (megakaryocytes). Breakdown and regeneration of red blood cells usually go hand in hand. This ensures that there are always enough blood cells available.
The regular degradation of old erythrocytes is carried out by so-called scavenger cells (macrophages) in the spleen, and to a lesser extent also in the liver. They dissolve and break down the coating of the red blood cells. Macrophages are found in different tissues, and doctors call them the “reticuloendothelial system”.
Erythrocytes have the task of binding oxygen to themselves and supplying it to the entire body. The main component of red blood cells is the red blood pigment hemoglobin. When the blood cell breaks down, the hemoglobin is broken down. The breakdown product bilirubin is formed, which enters the bile via the liver and is excreted from there in the stool and, to a lesser extent, in the urine.
In hemolytic anemia, more red blood cells break down than usual, while the bone marrow lags behind in producing new cells. The result is that there are too few erythrocytes overall.
The liver is overwhelmed by the increased breakdown of red blood cells: so many breakdown products such as bilirubin accumulate that they are no longer excreted quickly enough with the stool (and to a lesser extent with the urine). Instead, bilirubin accumulates in the mucous membranes and skin. This leads to the typical yellowing of the skin and mucous membranes.
What is anemia?
One speaks of anemia (low blood count) when the number of red blood cells (and thus also the red blood pigment haemoglobin) is below the age- and gender-specific reference value.
Anemia has many different causes: It is caused either by rapid breakdown of the red blood cells (hemolysis), enzyme or membrane defects in the blood cells, a distribution disorder (e.g. pregnancy anemia or hypersplenism due to an enlarged spleen) or by an autoimmune reaction in which the immune system mistakenly Forms defense bodies (antibodies) against red blood cells. Other causes of anemia are certain chronic diseases or cancers.
Course of the disease and prognosis
Both the course and prognosis of hemolytic anemia depend on the underlying cause.
For example, autoimmune hemolytic anemias have a good prognosis, especially after the spleen has been removed. The same applies to congenital spherical cell anemia: after removal of the spleen, the symptoms of the disease improve significantly. Overall, the treatment of congenital anemia has improved significantly over the past few decades. Secondary diseases and complications are largely manageable, and life expectancy has risen sharply. Elderly patients with additional cardiovascular diseases in particular have a less favorable prognosis.
In any case, it is important to have regular check-ups. In chronic hemolysis, the doctor closely examines the blood.
What are the symptoms of hemolytic anemia?
There are different causes of hemolytic anemia. Which symptoms occur depends on the trigger of the disease.
What they all have in common are the symptoms that are triggered by the excessive decay and degradation of the erythrocytes. Its severity depends on how quickly the anemia develops: the faster, the more pronounced the symptoms. If the anemia is congenital or develops slowly, the body adapts to the anemia and sometimes develops no or only weak symptoms.
The following symptoms indicate hemolytic anemia:
- Paleness
- Fatigue
- Derating
- Low blood pressure (hypotension)
- Dizziness
- Headache
- Tinnitus
- Circulatory problems to the point of fainting
- Palpitations
- Difficulty breathing
- Yellowing of the mucous membranes and skin (icterus): Caused by the breakdown of the red blood pigment (hemoglobin) contained in the red blood cells. The yellowish color is caused by bilirubin, the breakdown product of hemoglobin.
- Enlargement of the spleen (splenomegaly).
Possible complications of hemolytic anemia
Hemolytic Crisis: A hemolytic crisis occurs when a large number of red blood cells break down in a short period of time. Such crises are possible with favism, sickle cell anemia and blood transfusions. Signs of a hemolytic crisis are:
- Fever
- Chills
- Weakness
- Circulatory problems to the point of shock
- Stomach pain
- Back pain
- Headache
- Red or red-brown urine (if hemoglobin is excreted in the urine)
- Later yellowing of the mucous membranes and skin.
A hemolytic crisis is a medical emergency. Call an ambulance at the first sign!
Gallstones : Gallstones form in some patients as a result of chronic hemolytic anemia. They arise because the breakdown of the red blood pigment (haemoglobin) produces more bilirubin. It collects in the gallbladder and forms what are known as “pigment stones” in some patients.
Folic acid deficiency : In order to form new, healthy red blood cells, the bone marrow needs folic acid. A permanently increased formation of new erythrocytes may lead to a folic acid deficiency in the long term.
Iron deficiency: If too many red blood cells are lost, long-term iron deficiency occurs. Iron is a component of the red blood pigment hemoglobin.
Cause and risk factors
Corpuscular hemolytic anemia
In the case of corpuscular hemolytic anemia, the cause lies in the red blood cells themselves. This form of hemolytic anemia is usually inherited and manifests itself in childhood or adolescence. Here, different defects in the blood cells trigger haemolytic anemia:
- Congenital cell membrane disorder: globule cell anemia (hereditary spherocytosis)
- Acquired cell membrane disorder: paroxysmal nocturnal hemoglobinuria
- Erythrocyte metabolism disorder: favism (glucose-6-phosphate dehydrogenase deficiency)
- Hemoglobinopathy: sickle cell disease, thalassemia.
Extracorpuscular hemolytic anemias
In the case of extracorpuscular anemias, the cause does not lie in the red blood cells themselves, but in external factors. This form of hemolytic anemia is not usually congenital, but only develops over the course of life.
Possible causes are:
- Medications: Some active ingredients such as quinine and mefloquine (antimalarials), penicillin, antibiotics such as metronidazole, psychotropic drugs such as bupropion or painkillers (NSAID) such as ibuprofen may trigger haemolytic anemia.
- Autoimmune diseases: In an autoimmune disease, the immune system mistakenly forms defense bodies (antibodies) against harmless endogenous substances such as red blood cells. Examples include immune thrombocytopenia (ITP) and cold-type autoimmune hemolytic anemia.
- Infections: In some cases, infections cause hemolytic anemia. The most common pathogens include Clostridium perfringens, streptococci, meningococci, plasmodia, bartonella, Epstein-Barr virus and mycoplasma.
- Mechanical injuries to the erythrocytes: Here the red blood cells are damaged and destroyed by mechanical obstacles in the bloodstream (e.g. artificial heart valves).
- Enlargement and increased activity of the spleen (hypersplenism): When the spleen enlarges, more blood cells are broken down.
- Poisons (toxins): Poisoning with lead or copper leads to an increased breakdown of red blood cells.
- Drugs: Drugs such as ecstasy or cocaine can trigger hemolytic anemia.
Examination and diagnosis
Congenital hemolytic anemias such as sickle cell anemia or spherical cell anemia are usually diagnosed in childhood or adolescence. In many cases, doctors discover acquired anemias only by chance during blood tests, for example during a preventive medical check-up. In the case of already advanced hemolytic anemia, the yellowing of the skin or blood in the urine is usually the reason for the first visit to the doctor. Depending on the age of the patient, the first point of contact is the pediatrician or family doctor.
Medical history
In the first consultation, the doctor asks about the current symptoms and asks how long they have been present. If there is a suspicion of haemolytic anemia based on a blood test, the doctor will ask about other abnormalities. These include:
- Family history: Is there a family history of hemolytic anemia (such as thalassemia, sickle cell anemia, or favism)?
- Do you have a fever or other symptoms?
- Is the patient taking medication? If yes, which?
- Does the patient take drugs? If so, which ones (particularly cocaine)?
Blood test
If there is no current blood test, the doctor takes blood from the patient and pays particular attention to the following values:
- Decreased number of red blood cells (erythrocytes) and red blood pigment (haemoglobin)
- Increased number of reticulocytes (reticulocytosis, progenitor cells of the red blood cells in the bone marrow)
- Low haptoglobin (transport protein for the red blood pigment hemoglobin)
- Elevated bilirubin (bile pigment, sign of increased hemoglobin breakdown)
- Elevated LDH (sign of increased cell breakdown)
- Folic acid or iron deficiency.
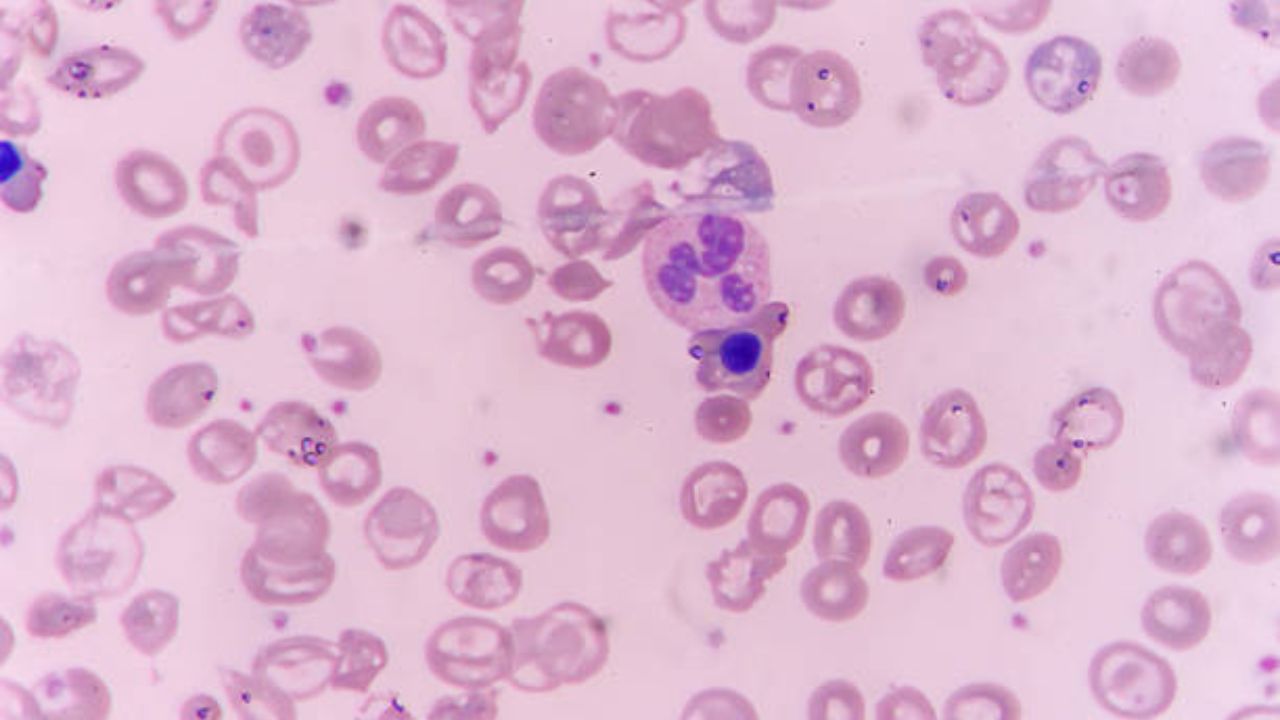
Blood smear
For a blood smear, the doctor puts a drop of blood on a glass slide and examines the individual blood cells under the microscope for changes. Certain changes in the shape of red blood cells provide clues to specific diseases that trigger hemolytic anemia. For example, in globular cell anemia, the erythrocytes are spherical instead of flat.
Urine test
The main part of the red blood pigment – or its breakdown product bilirubin – is excreted in the stool, a small part in the urine. If there is bilirubin in the urine, this is a sign of increased breakdown of red blood cells. Doctors speak of “urobilinogen”.
Coombs test
The Coombs test is a blood test to detect antibodies against erythrocytes. The doctor uses this to check whether the patient’s blood contains antibodies against the red blood cells.
Ultrasound examination
An ultrasound scan of the abdomen provides information about whether the spleen and/or liver are enlarged.
Treatment
How doctors treat hemolytic anemia depends on the underlying cause. Regardless of the cause of the disease, the goal of treatment is to resolve the anemia and control the disease.
Glucocorticoids and immunosuppressants: Glucocorticoids (cortisone) and immunosuppressants (medications that suppress an excessive reaction of the body’s own defense system) help in autoimmune hemolytic anemias.
Removal of the spleen (splenectomy): When the spleen is removed, fewer red blood cells are broken down. This helps relieve symptoms but makes sufferers more susceptible to infections. For this reason, patients are vaccinated against certain diseases (such as influenza, pneumococcal, meningococcal and Haemophilus influenzae infections) a few weeks before the operation.
Avoidance of triggering medication: If the cause of the haemolytic anemia is a specific active ingredient, the doctor will change the medication and, if necessary, switch to another, equivalent preparation.
Folic acid: In hemolytic anemia, the body needs more folic acid to stimulate the formation of new red blood cells in the bone marrow. Doctors recommend a folate-rich diet that includes spinach, lettuce, cabbage, fruit, whole grains, wheat germ, soybeans, legumes, and liver. If this is not enough, taking a folic acid supplement makes sense.
Bone marrow transplantation: Sickle cell anemia and thalassemia can be cured with bone marrow transplantation. Bone marrow is transferred from a healthy donor to the patient.
Phototherapy: Phototherapy may help infants born with favism or rhesus intolerance. The babies are irradiated with short-wave light, which converts the bilirubin in the skin and then excreted through the bile and kidneys.
Protection from cold: In the case of chronic autoimmune hemolytic anemia of the cold type, the most important measure is to protect those affected from the cold.
Prevention
Since haemolytic anemia has various causes, it can only be prevented to a limited extent. In any case, it is important to counteract nutritional deficiency symptoms. Eat a balanced diet and consume enough folic acid – found in spinach, beans, cabbage and liver. The same applies to vitamin B12 : it is found in fish, dairy products, meat and eggs. Doctors recommend that women eat iron-rich foods during menstruation. Red meat, whole grain products, legumes and nuts are ideal.
