Doctors refer to enlarged pharyngeal tonsils, which usually occur in childhood, as adenoids. If the adenoid is very large, it narrows the nasopharynx, so that affected children are no longer able to breathe through their nose. Read here what consequential damage occurs and how adenoids are treated!
ICD codes for Adenoids disease: J35
Quick overview
- What are adenoids? Adenoids is the name for enlarged pharyngeal tonsils. They mainly occur in children and, if left untreated, often cause serious consequential damage such as misaligned jaws and hearing loss.
- Symptoms: breathing through the mouth, breathing disorders during sleep, runny nose, frequent infections of the upper respiratory tract, middle ear infection, hearing loss, impaired speech development, misaligned jaws, misaligned teeth.
- Causes: Permanent inflammation due to recurring respiratory infections in childhood.
- Risk factors: Adenoids occur more frequently in some families (familial aggregation).
- Diagnostics: Typical symptoms, nasal reflection, examination of the ears, hearing test, biopsy (only for adults).
- Treatment: Surgery is usually necessary. After removal of the pharyngeal tonsils, the symptoms quickly subside. In rare cases, the adenoids grow back.
- Prevention: No prevention possible.
What are adenoids?
Adenoids is the name for enlarged pharyngeal tonsils. Doctors also speak of “adenoid vegetation” or pharyngeal tonsil hyperplasia.
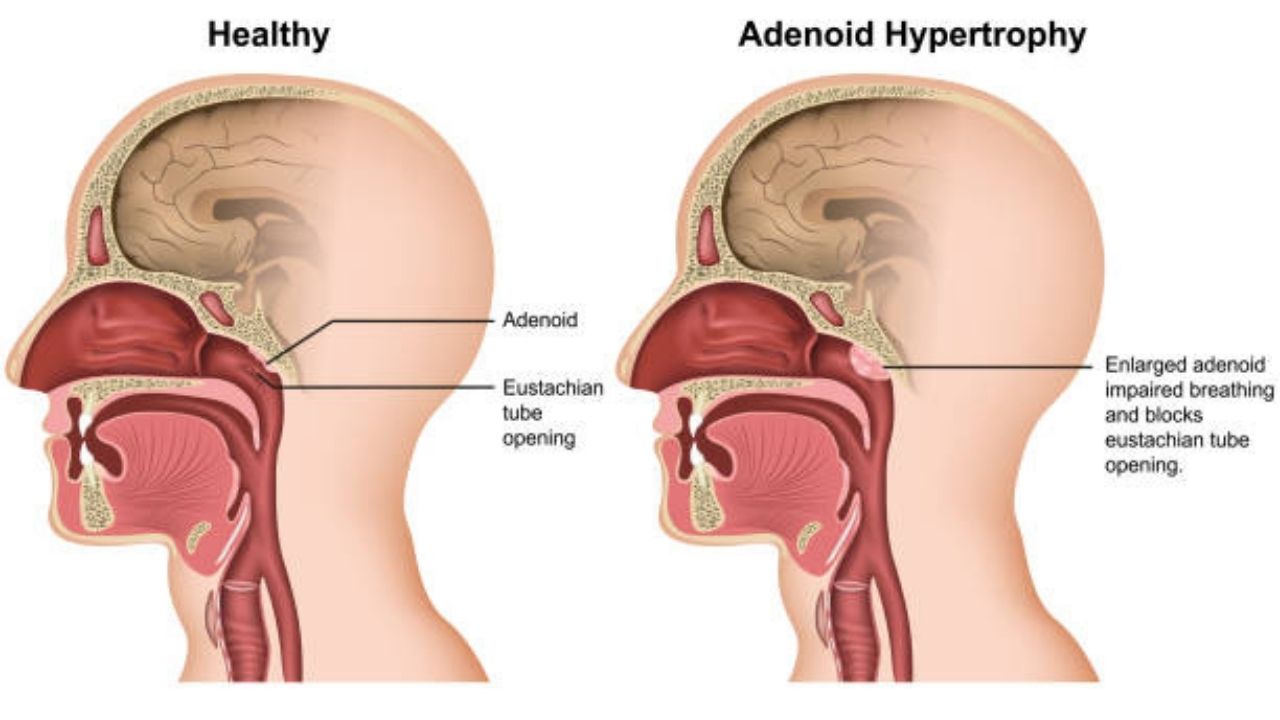
The pharyngeal tonsil is located in the middle of the back pharyngeal wall, the so-called pharyngeal roof. Unlike the tonsils, they are not visible when the mouth is open. Together with the lingual tonsil and the two palatine tonsils, the pharyngeal tonsil is responsible for fighting off pathogens that enter the body through the nose or mouth. They consist of lymphatic tissue and are therefore part of the immune system. Normally, the adenoids are about the size of a blackberry.
Since children’s immune systems are not yet fully developed, they often suffer from respiratory infections – the immune system in the throat is then running at full speed. The tonsils are often permanently enlarged and have no opportunity to return to their normal size. This is a problem especially in children between the ages of two and six, since the child’s nose and throat area is cramped anyway.
However, an adenoid only has disease status when symptoms occur. This is the case when the enlarged tonsil blocks the opening to the nasal cavity and/or the entrance to the middle ear. Affected children no longer breathe through their nose and may suffer permanent ear damage.
Some clinics classify adenoids into three grades of severity based on how much they narrow (block) the nasopharynx:
- Grade 1: Nasal cavity free.
- Grade 2: nasal cavity partially obstructed.
- Grade 3: nasal cavity completely obstructed.
Who is affected?
Adenoids usually appear between the ages of two and six, more rarely earlier or up to puberty. After puberty, they usually slowly regress. Adults only have very small tonsils, the pharyngeal tonsils have almost completely disappeared. Since physical growth also means that the space in the throat is no longer so cramped, adenoids are extremely rare in adults.
Adenoids or Polyps?
Enlarged tonsils are often mistakenly referred to as polyps. Real polyps, however, are mucous membrane growths in the paranasal sinuses (polyposis nasi), which usually only occur in adults.
Are Adenoids Dangerous?
If the pharyngeal tonsil is only enlarged without causing any symptoms, it does not pose a risk. It heals with age and shrinks on its own after puberty.
Adenoids that are greatly enlarged and block the opening to the nasal cavity or the entrance to the middle ear can cause serious consequential damage if left untreated.
These include:
Limited hearing: In the nasopharynx there is an open connection between the pharynx and the middle ear, the so-called Eustachian tube. If the entrance to this in the pharynx is closed by the enlarged pharyngeal tonsil, the middle ear is no longer ventilated. A permanent negative pressure is created in the ear, a feeling that is familiar from flying, for example.
Due to the negative pressure, fluid collects in the middle ear, which means that the eardrum does not transmit the sound waves as usual. Conductive hearing loss develops, which severely limits hearing.
Language development disorders: If the hearing impairment goes unnoticed for a long time, it often leads to language development disorders in children who are just learning to speak. These are often difficult to compensate for later in life.
Frequent middle ear infections: Another effect of the negative pressure in the ear is frequently recurring, sometimes very painful middle ear infections.
Frequent respiratory infections: The mucous membranes in the nose, mouth and throat play an important role in defending against pathogens. The permanent mouth breathing causes the mucous membranes to dry out and the filter function of the nose is no longer available. As a result, affected children are significantly more susceptible to colds and other respiratory infections.
Breathing pauses: Children who breathe through their mouth usually sleep restlessly and snore. In extreme cases, breathing stops (sleep apnea).
Malformations in the upper jaw and misaligned teeth: The constantly open mouth disturbs the normal growth of the upper jaw and causes misaligned teeth in the long term. A high, pointed palate typically develops.
Prognosis after surgery
After removal of the adenoids, the prognosis is good: the symptoms usually improve immediately after the procedure, 70 percent of all children are symptom-free in the long term. In rare cases, the adenoids (unlike the tonsils) grow back and require further surgery. Important to know: The pharyngeal tonsils are involved in the defense against disease in the nasopharynx, but not as important as the palatine tonsils. If the enlarged tonsils are removed, this has no disadvantages for the child’s immune system.
Symptoms of Adenoids
Many children live with an enlarged tonsil without showing any symptoms. Symptoms only arise when the adenoid is so large that it narrows the opening to the nasal cavity or the connection to the middle ear.
Typical symptoms are:
- Constant mouth breathing.
- Frequent sniffles.
- Snoring and pauses in breathing during sleep.
- Restless sleep.
- Persistent stuffy nose.
- Nasal speaking.
- Characteristic facial expression (Facies adenoidea): narrow pale face, mouth open, tongue is visible, eyes are slightly set back.
Children often do not notice an enlarged adenoid themselves, since it does not cause pain and over time they have become accustomed to constantly breathing through their mouth.
Causes of Adenoids
The cause of adenoids is not fully understood. Doctors assume that recurring respiratory infections cause the immune system, and thus also the adenoids, to run at full speed. The permanent inflammation prevents the natural regression of the pharyngeal tonsils. Doctors speak of a “circus vitiosus”: A “vicious circle” of inflammation, enlargement and renewed inflammation.
Risk factors of Adenoids
Adenoids are more common in some families. Doctors assume that affected families carry a certain predisposition.
What does the doctor?
If the child suffers from repeated respiratory infections, the first step is to see a pediatrician. During the first consultation, he or she will inquire about existing complaints and examine the child. Abnormalities such as nasal speech, snoring or a facial expression typical of adenoids with an open mouth and visible tongue (Facies adenoidea) give the doctor the first indications of the diagnosis “enlarged adenoids”. For further examinations, he refers the child to a specialist in ear, nose and throat medicine (ENT doctor).
Reflection of the rear nasopharynx (postrhinoscopy): The pharyngeal tonsil – even if it is enlarged – is not visible through the open mouth. To examine them, the doctor performs a nasal endoscopy. To do this, he presses the tongue down with a spatula and inserts an angled mirror over the mouth. If the pharyngeal tonsil is greatly enlarged, it appears as a reddish, lobed, longitudinally furrowed structure.
Examination of the ear: The doctor then checks whether there is a tympanic effusion (accumulation of fluid in the ear). For this he uses an otoscope; an instrument with which he looks at the external auditory canal and the eardrum.
Hearing test: If a hearing disorder is suspected, a hearing test is necessary.
Biopsy: A tissue sample is usually only taken from adults. To do this, the doctor removes a small piece of the changed tissue under local anesthesia and examines it under the microscope for changes. This is necessary to distinguish the adenoid from a malignant tumor, which is very rare in adults.
Treatment of Adenoids
Wait
In mild cases, the doctor advises you to wait and see. In some cases, the adenoids and the associated symptoms regress on their own. This is especially true for children who are approaching puberty. Parents are advised to pay attention to whether the symptoms are getting worse and, if necessary, to consult the attending ENT doctor soon.
Surgery
If the adenoid causes symptoms, an operation is usually necessary. It is important that the child is healthy on the day of the operation and has no infection. Otherwise, the doctor will postpone the procedure.
The operation is performed either directly in the practice of the ENT doctor or on an outpatient basis in the hospital. Since the procedure only takes about 20 minutes, short anesthesia is sufficient. The doctor removes the pharyngeal tonsils (adenotomy) with a special instrument (Beckmann’s ring knife) through the open mouth. The removal of the pharyngeal tonsils is very low-risk and therefore also possible in small children. The risk of secondary bleeding is also significantly lower than, for example, with tonsil surgery.
If there is fluid in the middle ear, the doctor sucks it out through a small incision in the eardrum (paracentesis). Under certain circumstances, he inserts a small tube (tympanic tube) into the eardrum so that the ear is better ventilated and the negative pressure escapes.
After the operation
Four to six hours after the operation, the doctor checks the operation site again for bleeding. If none are available, the child may leave the practice or the hospital again.
Tips for the time after the operation:
Watch out for secondary bleeding: secondary bleeding occurs only rarely, but quickly leads to a large loss of blood, since the tonsils are particularly well supplied with blood. It is therefore important not to leave the child alone, especially in the first 24 hours, and to keep a close eye on it. Bleeding may not be immediately obvious because blood does not always drip from the mouth or nose: children tend to swallow blood. If the child swallows conspicuously often, this is a warning sign of possible bleeding.
If you suspect bleeding, take your child to the hospital immediately or call an emergency service on the emergency number 112!
No physical exertion: No physical exertion and no wild romping for three to five days.
Grooming: No hot showers or baths for three to five days. If a ventilation tube has been inserted, no water should get into the ear!
School: Five to seven days after the operation, the child can go back to school or kindergarten. It can only take part in school sports again after two weeks!
Eating/drinking: In the first few days after the operation, it is possible that you may have difficulty swallowing. Soft, mushy and cool foods are particularly suitable. Hard foods such as bread crusts irritate the healing tissue and may cause bleeding. Also, make sure your child is drinking enough.
Check-up: If the doctor treating you does not recommend a different (possibly earlier) appointment, the routine check-up will take place on the eighth day after the operation.
Painkillers: If the child suffers from pain after the operation, give your child painkillers as an exception – but only after consulting the doctor. Active ingredients such as ibuprofen or paracetamol are available in child-friendly dosages. Talk to the doctor treating you about it.
Healing: It takes two to three weeks for the surgical wound to heal completely.
Other: Smoke irritates the mucous membranes and interferes with wound healing. Therefore, make sure you are in a smoke-free environment. Sleeping with your head slightly elevated makes breathing easier.
Medication
Decongestant nasal sprays or nasal drops are not recommended for adenoids because they only work for a short time and do not eliminate the cause. The doctor only prescribes antibiotics (medicines against bacterial infections) in exceptional cases, since respiratory tract infections are usually caused by viruses .
Prevention of Adenoids
Prevention of adenoids is not possible. Many children have enlarged tonsils by school age. It is impossible to predict which child will actually suffer from the symptoms. If adenoids are known in the family, it is advisable to pay more attention to the typical symptoms.
