Bacterial vaginosis for men – Bacterial vaginosis (BV) is an imbalance in the composition of the bacteria that naturally live in the vagina. Males can’t get bacterial vaginosis because the penis doesn’t have the same delicate balance of bacteria, but they can spread the infection.
Bacterial vaginosis – also known as Gardnerella infection, Haemophilus vaginalis infection or amine colpitis – is what doctors call a pathological imbalance in the vaginal flora. It is caused by increased colonization of the vagina with the bacterial species Gardnerella vaginalis and other germs. Bacterial vaginosis typically manifests itself as increased discharge that has an unpleasant, fishy odor. Bacterial vaginosis is usually treated with antibiotics and/or lactic acid preparations.
ICD codes for this disease: N76.0
Causes – How does bacterial vaginosis develop?
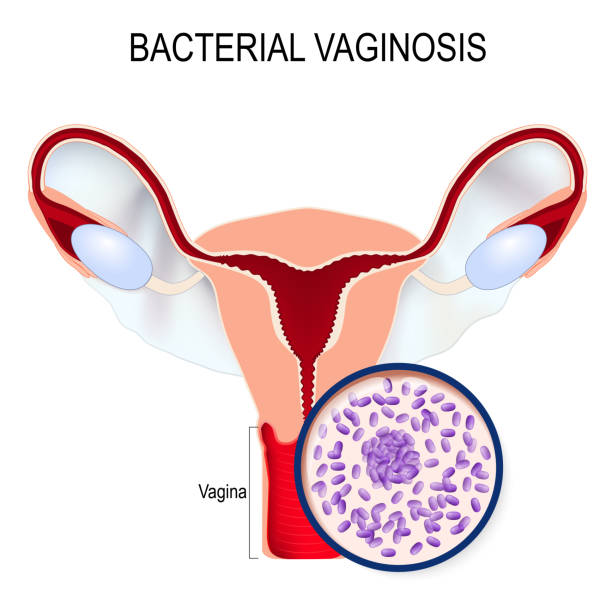
The healthy, normal vaginal flora of a sexually mature woman consists mainly of different types of lactic acid bacteria (lactobacilli). These normally ensure an acidic environment in the vagina with a pH value of 3.8 to 4.4 and thus suppress the multiplication of disease-causing germs.
In the case of bacterial vaginosis, however, the “good” lactic acid bacteria are displaced by pathogenic germs, mainly the bacterial species Gardnerella vaginalis, but also chlamydia, mycoplasma and Bacteroides bacteria.
This leads to an excessive colonization of the vagina with pathogenic bacteria, while the number of lactic acid-producing lactobacilli decreases. The pH value of the vaginal flora then rises to around 5, as the healthy acidity of the vagina decreases and the vaginal environment becomes imbalanced. The clinical picture “bacterial vaginosis” is then present.
Risk factors are in particular incorrect vaginal hygiene. Below you can find out how you can prevent the disease.
Symptoms – How does bacterial vaginosis manifest itself?
Bacterial vaginosis does not necessarily cause symptoms. Bacterial vaginosis is asymptomatic in about 40 to 50 percent of cases, ie the affected women are symptom-free.
Otherwise, about half of the affected women complain of increased, thin, sometimes foamy vaginal discharge (fluor vaginalis). This is characterized by a gray-whitish to yellowish color and usually has an unpleasant, fishy, sometimes sweet smell. In some cases, the unpleasant fishy odor occurs even without the accompanying discharge.
Other women, on the other hand, report an increased discharge, while the fishy smell is missing. Above all, the fishy intimate odor is perceived as very stressful and unpleasant by the women affected. It has nothing to do with a lack of intimate hygiene, but rather arises from the fact that the causative pathogens of bacterial vaginosis break down certain proteins into so-called amines.
Complaints such as itching, burning, redness and skin irritation in the outer vaginal area are rather atypical for bacterial vaginosis, but can also occur in rare cases. In addition, symptoms such as mild stabbing pain and problems with sexual intercourse or urination are also possible.
Diagnosis of bacterial vaginosis
By definition, the diagnosis of “bacterial vaginosis” is confirmed if at least three of the following four findings can be obtained during a gynecological examination:
• An increased thin liquid to foamy and gray-whitish to yellow homogeneous vaginal discharge (fluor vaginalis) occurs.
• The pH of the vaginal flora (vaginal flora) is greater than 4.5.
• The vaginal discharge smells fishy (amine smell).
• In the native preparation (smear of the vagina), so-called key cells (clue cells) can be detected under the microscope in at least 20 percent of the vaginal cells.
To collect these findings, the attending gynecologist takes a swab from the woman’s vagina as part of the gynecological examination and then carries out a series of tests and examinations.
This includes the pH test, the so-called amine test, the cytological test under the microscope to assess the vaginal cells and the creation of a bacterial culture.
pH testing to diagnose bacterial vaginosis
The pH value can be easily checked with tweezers and a pH indicator strip. In addition, there are also special gloves available in pharmacies that make it easy to determine the pH at home.
Amine test to diagnose bacterial vaginosis
With the so-called amine test, also known as the “whiff test”, the fishy smell (amine smell) of the vaginal discharge (fluor vaginalis) that occurs with bacterial vaginosis can be better assessed. To do this, the doctor first takes a swab from the vagina.
He then drips one or two drops of a ten percent potassium hydroxide solution onto the swab material. The typical fishy smell of the vaginal discharge is intensified by the potassium hydroxide so that the doctor can better draw conclusions about the presence of bacterial vaginosis.
Cytological examination to diagnose bacterial vaginosis
As part of the cytological examination, the native preparation, consisting of swab material from the vagina, is examined under the microscope. If so-called key cells (clue cells) can be detected under the microscope in at least 20 percent of the vaginal cells (vaginal epithelial cells), this indicates bacterial vaginosis. The key cells are cells covered with bacteria, which can be seen under the microscope as small granules.
The microscopic examination can also be used to assess the number of bacteria and whether the colonization is a mixed infection with different types of bacteria.
The cytological examination can only make a suspected diagnosis of “bacterial vaginosis”. Further investigations are necessary for a definite diagnosis. This includes, for example, the creation of a bacterial culture.
Creating a bacterial culture
With the help of a bacterial culture, the causative agent of bacterial vaginosis can be clearly detected and determined. It is usually applied if bacterial vaginosis recurs regularly (stubborn recurrences) or if it is to be checked whether other microorganisms are responsible for the symptoms.
Differential diagnostics
As part of the differential diagnosis, it should be ensured that it is actually bacterial vaginosis and that the symptoms are not the result of other diseases that cause similar symptoms. The diagnosis should include, among other things, differentiation from vaginal inflammation (vaginitis) and inflammation of the mucous membrane of the cervix (cervicitis). In addition, infection with other microorganisms such as trichomonads or mycoplasma should be ruled out.
Treatment of bacterial vaginosis
Only the detection of the bacterial species Gardnerella vaginalis or other anaerobic bacteria in the vaginal flora does not make treatment necessary. Therapy should only be carried out when the affected woman suffers from symptoms such as increased discharge and the typical fishy odor in the genital area and the diagnosis is confirmed.
Bacterial vaginosis is not a serious condition. However, it should always be treated, since the symptoms are very unpleasant for the women affected and sometimes there are also complications, ie serious illnesses such as inflammation
• The lining of the cervix (cervicitis).
• The lining of the uterus (endometritis).
• The fallopian tubes (salpingitis).
• Of the vaginal entrance (vulvitis) or
• The Bartholin glands (Bartholinitis),
can entail.
Bacterial vaginosis is usually treated with antibiotics. In addition, preparations containing lactic acid bacteria can also be used, which have a positive effect on the imbalance in the vaginal flora present in bacterial vaginosis.
Treatment with antibiotics
The administration of antibiotics represents the gold standard in drug therapy for bacterial vaginosis. The antibiotic metronidazole in particular has proven to be very successful, as it is particularly effective against anaerobic bacteria. Other active ingredients are also available. These include clindamycin, amoxicillin or nifuratel.
The antibiotics can be administered either orally in the form of tablets (metronidazole) or intravaginally in the form of vaginal suppositories or vaginal tablets. Topical treatment with an antibiotic vaginal cream (metronidazole, clindamycin) is also possible.
How long and how intensively bacterial vaginosis is treated with the antibiotics mentioned depends on the severity of the disease and the ability of the vaginal flora to regenerate.
Treatment with lactic acid preparations
As an alternative to treatment with antibiotics, local treatments with preparations containing lactic acid and vaginal suppositories containing lactic acid bacteria (lactobacilli) or ascorbic acid (vitamin C) are also possible for bacterial vaginosis.
Treatment with lactic acid, lactobacillus and ascorbic acid preparations, which are now available in pharmacies without a prescription, serves to rebuild the natural vaginal environment. However, it succeeds neither as quickly nor as thoroughly as the treatment of bacterial vaginosis with antibiotics. For this reason, preparations of lactic acid, lactobacillus and ascorbic acid are mainly used after treatment with antibiotics to support the healing achieved and to prevent bacterial vaginosis from recurring.
Bacterial vaginosis prognosis
If bacterial vaginosis is treated with antibiotics, the overall prognosis is good. Bacterial vaginosis usually heals within a week with antibiotics. Normal vaginal flora is restored after a week after oral administration of metronidazole and 80 percent of the patients are cured. Similarly good results are obtained with the intravaginal administration of metronidazole.
However, the relapse rate after successful treatment is quite high at 60 to 70 percent. Simultaneous treatment of the partners of affected women can possibly prevent recurrences.
Bacterial vaginosis in pregnancy
Bacterial vaginosis can lead to various complications in pregnant women. For example, pregnant women who suffer from bacterial vaginosis have an increased risk of suffering premature labour, premature rupture of the amniotic sac or premature birth. In addition, infection of the embryonic envelope (amnionitis) can occur during pregnancy.
Various biochemical reactions between the fetus and the uterus, which are triggered by bacterial vaginosis, are responsible for these possible complications during pregnancy. After delivery, other complications may arise due to bacterial vaginosis. These include, among other things
• Inflammation and a delayed healing process of an episiotomy
• An abdominal wall abscess after a cesarean section
• Inflammation of the womb lining (endometritis).
Bacterial vaginosis should therefore always be treated medically during pregnancy. The treatment is the same as for non-pregnant women.
Frequency of bacterial vaginosis
Bacterial vaginosis is the most common microbiological disorder of the vaginal environment in sexually mature women. In Europe, bacterial vaginosis can affect 5 percent of women who come for a check-up and 30 percent of women who are treated in a clinic for sexually transmitted diseases, be detected.
About 7 to 22 percent of pregnant women in Europe are affected by bacterial vaginosis. Overall, around 20 percent of all women suffer from a bacterial vaginal infection, usually bacterial vaginosis, at least once in their lives.
Prevention of bacterial vaginosis
Preventing bacterial vaginosis is only possible indirectly. The general rule is: make regular check-up appointments with your gynaecologist ! This allows an existing bacterial vaginosis to be recognized and treated. The gynecologist can also intercept any complications that may arise.
Psychosocial stress is also considered a risk factor. Therefore, women with a lot of everyday stress should counteract this with sport and targeted relaxation techniques. Especially if you have had bacterial vaginosis before.
Important role in prevention: vaginal hygiene
Many women feel the need to clean their intimate areas thoroughly and use soap or shower gel and then intimate deodorant. This causes a fresh and pleasant feeling immediately afterwards, but this is only subjective and doesn’t last long. Excessive vaginal hygiene, such as vaginal douching, is particularly harmful! Regular care with just water is completely sufficient and it keeps the pH value of the vaginal flora at a constant level.
Chemical substances cause severe irritation in the vaginal flora, which disturbs its balance. In addition, many body care products have a high pH value, which throws the naturally acidic environment of the vaginal mucosa (low pH value) out of balance.
To prevent bacterial vaginosis, it is therefore important to carry out proper intimate hygiene using only lukewarm water or to use special washing lotions that are adapted to the pH value (< 5) of the vaginal environment. Special washing lotions are available in pharmacies or drugstores, for example. In order to regenerate the vaginal flora, to rebuild the colonization with the natural lactic acid bacteria (lactobacilli) and to stabilize the pH value over a longer period of time, the vaginal flora can be built up and acidified, for example, with special cures or lactic acid preparations.
Cleaning the anus and especially the wiping direction after a bowel movement can also contribute significantly to a healthy vaginal flora. Because with the right wiping direction from front to back (towards the anus and beyond), bacteria from the intestine are not accidentally introduced into the vagina.
Keep an eye on the pH of the vaginal flora
If you tend to have an acidic vaginal environment, you can also monitor this yourself using pH tests that are available without a prescription. So-called test sets can be bought in pharmacies as special pH indicator paper or pH test gloves. An explanation of pH can be seen on these products, with a vaginal pH above 4.5 (alkaline range) indicating a bad to abnormal change.
In such cases, the vaginal flora can be built up, for example, with lactic acid cures or lactic acid preparations.
Bacterial vaginosis sex
Bacterial vaginosis is not a sexually transmitted disease, but it can be promoted by sexual intercourse. Since the causative bacteria can also be present in the male genital area, but they do not cause any symptoms, the man can unknowingly pass them on to the woman. In this way, the woman can repeatedly come into contact with the bacteria. A comprehensive therapy therefore also includes the treatment of the sexual partner of the affected woman.
Since Gardnerella vaginalis is also an intestinal bacterium, it is often transmitted from the anal area to the vagina during sexual intercourse. In addition, switching from anal sex to vaginal intercourse increases the risk of introducing the intestinal bacterium Gardnerella vaginalis into the vagina. A condom also offers security here so that infection with bacterial vaginosis through sexual intercourse can be prevented. A fresh condom should be used, especially if you switch immediately from anal sex to vaginal intercourse.
Bacterial vaginosis for men
In men, too, the intimate area is often colonized with bacteria such as Gardnerella.
In these cases, however, the pathogenic germs usually do not cause any symptoms. The development of a mostly mild and short-lasting glans inflammation (balanoposthitis) is possible.