A colon with polyps (colon polyps) is a small lump in the inner lining of the large intestine, which can progress to cancer. They can occur with certain diseases or without any recognizable cause. In most cases, colon polyps do not cause any symptoms. They are discovered by accident during a colonoscopy. Because they can progress to colon cancer, doctors usually remove colon polyps. Read everything you need to know about colon polyps here.
ICD codes for colon polyps: K63 | C26 | D12
Brief overview: Colon polyps
• What are colon polyps? Mucosal growths that bulge into the intestine.
• Are colon polyps dangerous? In principle no, but there is a risk of degeneration into colon cancer.
• Frequency : One third of all people over the age of 60 have colon polyps.
• Symptoms : Very rare, mostly incidental findings during colonoscopy, possibly slimy or bloody stool, possibly stool changes.
• Diagnosis : Usually by colonoscopy.
• Treatment : Removal of the colon polyps (polypectomy), usually as part of a colonoscopy.
Colon with polyps: What are colon polyps?
Colon polyps are mucosal structures that protrude into the cavity of the intestine. They may sit flat on the intestinal mucosa, be attached to it by a style, or take on a “shaggy” shape.
Polyps are very common in the colon and rectum. They can be made of different fabrics. They mostly arise from glandular tissue of the intestinal mucosa. In this case, the colon polyps are called adenomas. Adenomas are benign structures that can transform into malignant cancerous tissue.
About 70 percent of colon polyps are adenomas!
After the age of seventy, almost half of all people in Europe carry at least one polyp in their intestines. A distinction is made between single polyps and diseases with several or numerous colon polyps. In a so-called polyposis there are countless polyps in the intestine. Symptoms are mostly diarrhea and abdominal cramps.
Types of colon polyps
Physicians distinguish colon polyps, which often form again in the intestine without any apparent cause (neoplastic intestinal polyps such as an adenoma), from polyps that are, for example, caused by inflammation (non-neoplastic colon polyps). The latter also include hamartomatous polyps. They arise from scattered germ cells and are usually congenital colon polyps.
If the upper mucosal cells multiply, doctors also speak of hyperplastic colon polyps. They are mostly small. Adenomas are typically larger. If colon with polyps (colon polyps) develop from fatty tissue cells, they are called lipomas. Under certain circumstances, a polyp is already degenerated – then colon cancer is present.
Symptoms of colon polyps
Many people ask the question: How do I spot colon polyps? Are there any specific symptoms? Polyps in the intestine usually do not cause any symptoms. Instead, doctors discover them by accident during a colonoscopy.
Use the cancer screening tests! colon polyps usually remain symptom-free, but in many cases increase the risk of colon cancer!
Blood in the stool
Occasionally, colon with polyps may bleed. The affected person sometimes notices this through reddish stools. Often the blood cannot be seen and can only be detected by special tests (e.g. immunological stool test (iFOBT)). However, polyps in the intestine rarely bleed permanently. However, they can cause symptoms of anemia such as dizziness and weakness.
Altered bowel movements
Sufferers may also have mucous stools. Diarrhea and abdominal cramps are also possible symptoms. In a few cases, colon polyps cause constipation.
Colon with polyps: Causes and risk factors
Colon polyps are much more common in the western world than, for example, in Asian countries. It is therefore assumed that the western lifestyle promotes the development of colon polyps. These include high-fat and high-sugar foods, alcohol consumption and nicotine.
Lack of exercise also likely plays a role in the development of colon polyps. Furthermore, genetic factors have a major influence.
Development of colon polyps
The lining of the colon regenerates itself regularly. Old mucosal cells are broken down and new cells multiply. They then form the new mucous membrane. This is a continuous process.
Small errors (mutations) in the genetic material can occur during reproduction. The body’s natural repair mechanisms usually correct these errors. From time to time, however, certain mutations change the growth properties of the mucosal cells.
Then they multiply excessively, for example. This causes colon polyps. If intestinal polyps persist for a long time, the damaged cells can degenerate – colon cancer develops. Therefore, doctors remove colon polyps preventively.
Colon with polyps: Genetic factors
Sometimes the tendency to form polyps in the gut can be inherited. Doctors distinguish a genetic predisposition without a proven cause from actual hereditary diseases. Colon polyps start growing much earlier in life. The risk of developing colon cancer is also increased.
Colon polyps in familial adenomatous polyposis (FAP)
In the rare case of familial adenomatous polyposis (FAP), polyps grow from the glandular tissue throughout the intestine (adenomatous colon polyps). An inherited genetic change is the cause. In some cases, however, the mutations also appear again.
Affected people usually have some colon polyps in their teens. However, polyps are often found elsewhere in FAP, such as in the stomach. Complaints are rather rare. Then abdominal pain, diarrhea, weight loss, flatulence or bloody-slimy bowel movements are possible.
If left untreated, they almost always develop into colon cancer. People who have family members with this condition should have their bowels checked regularly. In addition, relatives should be tested for FAP as part of genetic counseling.
Experts recommend that people suspected of having FAP have an annual recto-sigmoidoscopy (“small” colonoscopy) from the age of ten!
If colon polyps are found in the small colonoscopy of the rectum and the S-shaped section of intestine immediately in front of it, doctors reflect the entire intestine as a result. Thereafter, a yearly complete colonoscopy is advisable.
Irregular tooth structures or changes in the retinal pigmentation in the eye also occur with FAP. If those affected have tumors in their bones (e.g. osteomas) and other tissue (e.g. epidermoid cysts), doctors speak of the so-called Gardner syndrome, a special form of FAP.
The risk of developing thyroid cancer is also slightly increased. In addition to colon polyps, about 80 percent of FAP patients also have thyroid nodules. Growths in the liver are also possible.
MUTYH-associated polyposis (MAP)
In the case of MUTYH-associated polyposis (MAP), an inherited genetic defect is also the cause of early and frequent colon polyps. However, the disease is milder than FAP, fewer polyps develop, and they develop later in life.
The genetic defect is inherited in an autosomal recessive manner. This means parents can carry the mutated gene without being sick. If the father and mother each pass on a mutated gene, there is a risk that the offspring will become ill. Those affected have an 80 to 100 percent risk of developing colon cancer once in their lifetime.
Cronkhite Canada Syndrome
In the rare Cronkhite-Canada syndrome, colon polyps occur throughout the gastrointestinal tract. There are also brown spots on the skin. The structure of fingernails and toenails can change, and the hair on the head can fall out.
The syndrome usually occurs after the age of fifty. Severe diarrhea, which washes electrolytes and proteins out of the body, and threatening intestinal bleeding are problematic. In contrast to other genetic colon polyps, there is no higher risk of colon cancer here.
There is no specific treatment for Cronkhite-Canada syndrome. Sometimes, however, it responds to immune suppression therapy (immunosuppression).
Birt-Hogg-Dube Syndrome
In Birt-Hogg-Dube syndrome, numerous colon polyps occur in the large intestine, which very often can develop into colon cancer. In addition, tumors of the skin, kidneys and lungs occur.
Hamartomatous Polyposis Syndromes
A hamartomatous syndrome can be associated with growths in almost any part of the body. They arise from scattered germ tissue. These are cells from embryonic development. These cells are not structured like the normal intestinal mucosa.
If colon polyps occur as part of such a syndrome, the risk of colon cancer is increased. The disease usually appears at a young age. Examples of hamartomatous colon polyps are:
• Peutz-Jeghers syndrome : diagnosis around age 35; common polyps in the small intestine ; risk of colon cancer about 40 percent, increased risk of pancreatic cancer, breast cancer or ovarian cancer ; often pigment disorders in the mouth area.
• Familial juvenile polyposis : familial in about one third, risk of colorectal cancer about 20-70 percent.
• Cowden syndrome : many intestinal polyps, but also in the rest of the gastrointestinal tract, also growths on the skin, often thyroid diseases including cancer, high risk of breast cancer; increased risk of colon cancer.
Investigations and diagnosis of colon polyps
The first point of contact, for example in the event of problems with bowel movements, is the general practitioner. He usually also plans colon cancer screening. For this he will refer you to a gastrointestinal specialist (gastroenterologist).
Collection of medical history
The doctor first asks a few questions to get clues about his patient’s gut health:
• Do you or did you suffer from constipation, diarrhea or irregular bowel movements?
• Have you noticed your stool is bloody or mucous?
• Are there intestinal diseases in your family?
• Have you lost weight unintentionally in the last few weeks and months?
Physical examination
This is followed by the physical examination. With the stethoscope, the doctor can hear bowel sounds. Then he feels the abdomen for possible hardening. Colon polyps (colon with polyps) can sometimes be visualized in the rectum with an ultrasound machine.
The doctor can also feel intestinal polyps in the rectum. For this he leads a finger into the anus. This so-called digital rectal examination (DRE) is also common for prostate cancer screening in men. The doctor may also find signs of bleeding from bloody stool residue on the glove.
Colonoscopy
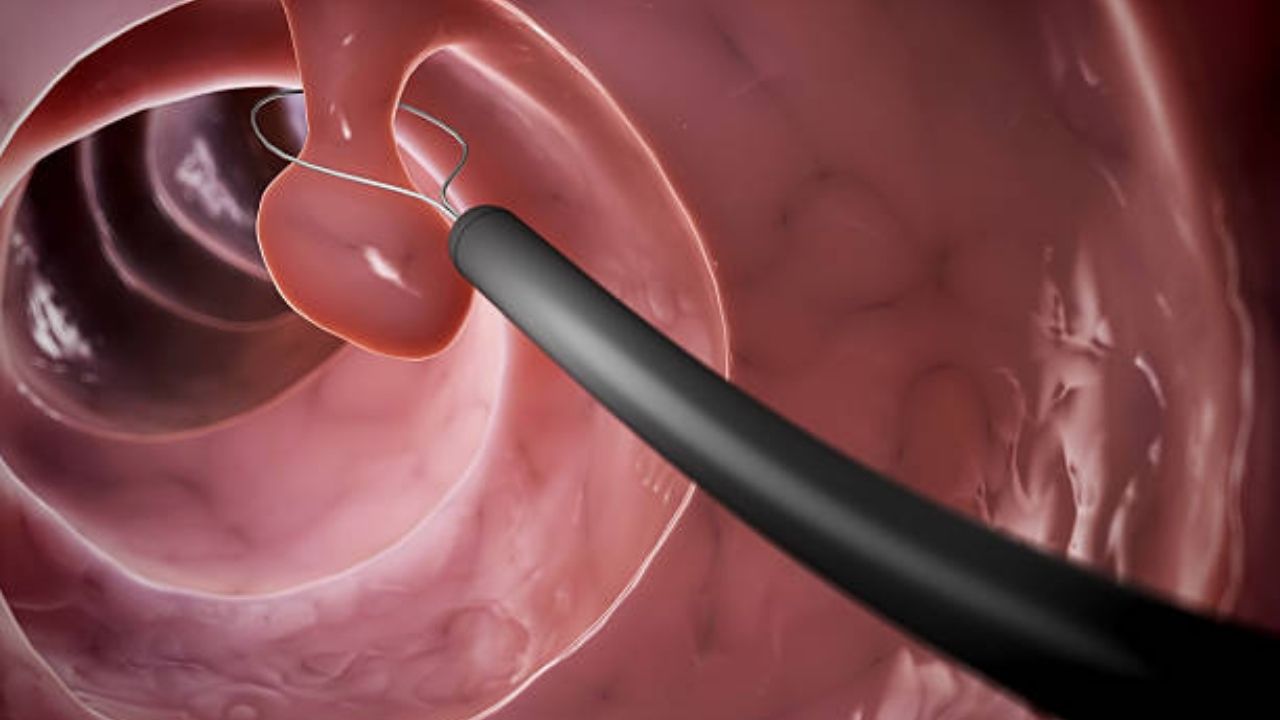
Colonoscopy is the most reliable method of detecting colon polyps. A flexible tube with a camera (endoscope, colonoscope) and light source is inserted into the intestine and advanced. If the doctor discovers a polyp in the intestine, he can remove it immediately.
Pathologists then examine the tissue. In doing so, they recognize exactly which intestinal polyp is present. Adenomas are divided into three subtypes. Depending on the type, the risk of the intestinal polyp developing into cancer varies:
• Tubular adenoma : most common form (60-65 percent), tubular growth, in the mirror you can see the intestinal polyps hanging on the intestinal wall like on a stalk, risk of degeneration about four percent.
• Villous adenoma : relatively rare (5-10 percent), widespread, looks like a turf in the mirror, about half of these colon polyps (colon with polyps) degenerate into colon cancer.
• Tubulovillous adenoma : about 20-25 percent of adenomas, mixed form of tubular and villous intestinal polyp.
Abdominal CT/MRI
If a colonoscopy is not possible, doctors can switch to a virtual colonoscopy. They take cross-sectional images using computed tomography (CT) or magnetic resonance imaging (MRI). However, as a rule, only intestinal polyps that are larger than one centimeter can be seen.
Video capsule endoscopy
In video capsule endoscopy, patients swallow a small capsule containing a camera. As it travels through the digestive tract, it takes pictures of the intestinal lining. This examination is very time-consuming and expensive. Usually, it only makes sense if other examination methods fail. On the other hand, it is important in the case of hereditary intestinal polyps, because it also takes pictures in the small intestine, which an endoscope cannot reach.
Prevention of colon polyps
Colon with polyps (colon polyps) and colon cancer are not uncommon diseases. For every person in European countries, the health insurance companies pay for check-ups from a certain age:
• From the age of 50 : annual stool test for hidden (occult) blood (immunological stool test (iFOBT).
• Men over 50, women over 55 : colonoscopy every ten years, if there are any abnormalities, the interval to the next colonoscopy is shortened.
• If the colonoscopy is rejected : every five years small endoscopy only up to the S-shaped bowel section and annual stool tests for occult blood.
If intestinal polyps accumulate in the family, doctors recommend colonoscopy more frequently and earlier. Exactly how often depends on the type of hereditary colon polyp (colon with polyps) or colon cancer.
If first-degree relatives (children, parents or siblings) have an adenoma before the age of 50, those affected should have an examination ten years before the age at which the relative developed the intestinal polyp.
Talk to your relatives! This is the only way you can better assess the risk of colon with polyps (colon polyps) and ultimately colon cancer!
If you then suspect a family history or even a hereditary disease, talk to a doctor you trust about it. He can direct you to specialists. Sometimes it is advisable to visit genetic counseling.
Treatment for Colon polyps
Since an intestinal polyp can progress to cancer, the doctor removes it – usually as part of a colonoscopy (polypectomy). How exactly he removes the intestinal polyp ultimately depends on its size:
The doctor usually removes intestinal polyps under five millimeters with biopsy forceps. For larger colon polyps, he uses an electric snare.
If the intestinal polyps sit broadly on the mucous membrane, a loop removal is hardly possible. Then the doctor performs a colonoscopy with a minor operation (transanal endoscopic microsurgery, TEM).
Large polyps sometimes need to be removed with surgery through the abdominal wall. In rare cases, surgeons remove an entire one. In people who suffer from a genetic polyposis and have a very high risk of colon cancer, the colon is sometimes operated on as a precautionary measure.
Course of the disease and prognosis
A polyp is actually a benign colon tumor. However, if it persists for a long time, it can develop into colon cancer. On average, it takes five to ten years for an adenoma to develop into colon cancer (adenoma-carcinoma sequence).
The larger the colon polyps, the greater the risk of colon cancer.
Tips for colon polyps
• Diet : Food high in fat, sugar and meat with little fiber, alcohol and nicotine promote the development of colon with polyps (colon polyps) and colon cancer. So make sure you eat a balanced diet.
• Exercise : Regular physical exercise helps keep your body fit. This also prevents colon polyps or colon cancer.
• Prevention : Also take advantage of the preventive medical check-ups that are offered. The health insurance companies cover the costs at certain intervals. Ideally, you should consult your family doctor.
• Control : If the doctor has removed intestinal polyps, ideally you should follow the advice of your doctor. If necessary, he will recommend an earlier check-up than after the usual ten years.
• Pre-existing conditions : Take extra care if your family has a pre- existing condition. Many intestinal polyps, but also chronic inflammatory bowel diseases such as ulcerative colitis or other malignant tumor diseases in the family ultimately increase your risk of colon cancer.
