The term leukemia refers to various cancers of the blood-forming system (“blood cancer”). What they all have in common is that degenerated white blood cells (leukocytes) multiply uncontrollably. The name itself suggests this: “Leukemia” means “white blood”. Read more about the symptoms, types, treatment, prognosis and what causes of leukemia here!
ICD codes for this disease: C91 | C95 | C93 | C92 | C94 | D47
Quick overview
• Symptoms: Tiredness and exhaustion, reduced performance, pale skin, tendency to bleed and bruises (haematomas), tendency to infections, fever of unknown cause, weight loss, night sweats.
• Common types: Acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), chronic myeloid leukemia (CML), chronic lymphocytic leukemia (CLL); actually a form of lymph node cancer)
• Treatment: Depending on the type and stage of the leukemia, options include chemotherapy, tyrosine kinase inhibitors, interferons, monoclonal antibodies, radiation therapy, and/or stem cell transplantation.
• Prognosis: Acute leukemia can often be cured if it is recognized and treated in good time. In the case of chronic leukemia, therapy may extend the survival time of many patients. Healing is only possible with a high-risk stem cell transplant.
• Diagnosis: The doctor takes the medical history and performs physical examinations. There are also ultrasound examinations, magnetic resonance imaging (MRI), computer tomography (CT), scintigraphy, blood tests, tissue samples (biopsy, spinal cord puncture) and examination of the spinal cord fluid (lumbar puncture).
• What causes of leukemia and risk factors: The causes are largely unclear. Risk factors are a genetic predisposition, age, smoking, exposure to radiation, chemical substances such as insecticides, some drugs (cytostatics), pathogens such as viruses.
• Prevention: There is little if any prevention of leukemia. However, a healthy lifestyle minimizes the risk of disease. With regular check-ups, for example, non-specific signs can be clarified in good time.
What is leukemia?
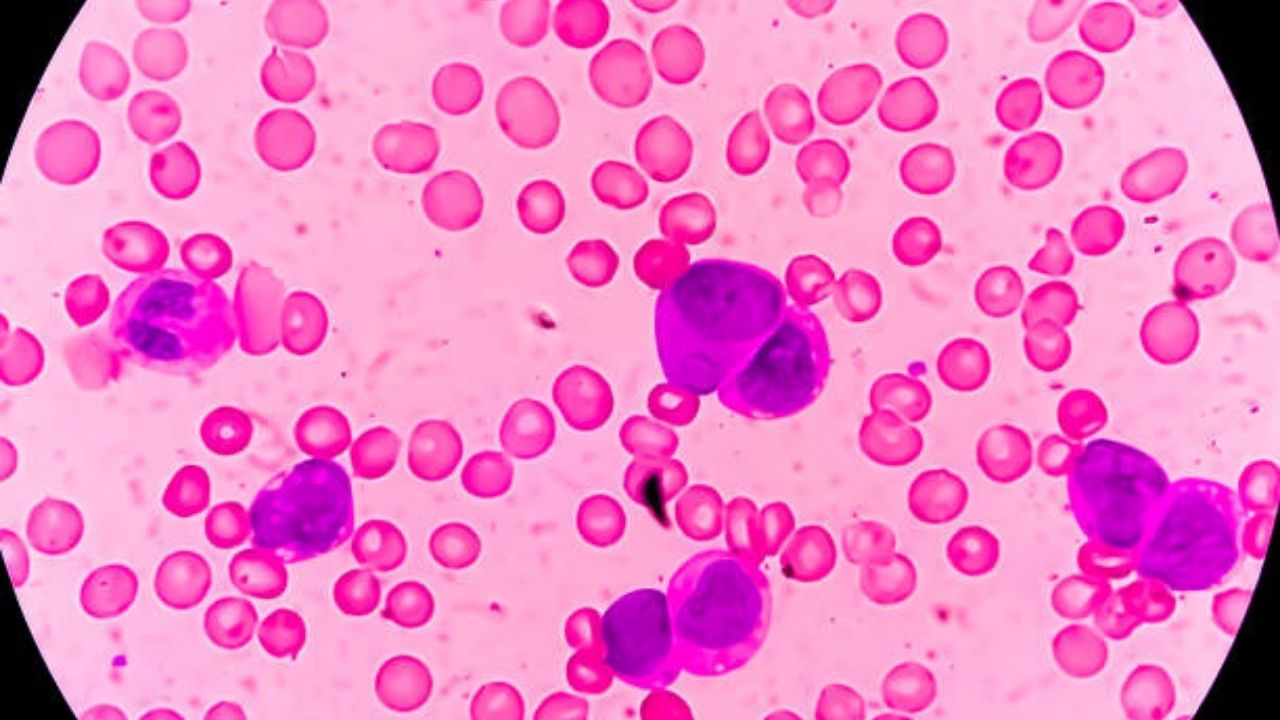
The term leukemia covers a group of cancers of the hematopoietic system – also called “blood cancer” or “leukosis”. Leukemia occurs when white blood cells (leukocytes), which arise from special stem cells in the bone marrow, develop incorrectly and then multiply uncontrollably. These leukocytes are not functional and, as the disease progresses, increasingly displace the healthy white and red blood cells (erythrocytes) and blood platelets (thrombocytes).
The development of blood cells takes place in stages, with each step initially producing a so-called immature progenitor cell. Each of the different types of white blood cells matures from its own progenitor cell. A disruption of this cell maturation is possible at each of the individual stages. Therefore, there are also different types of leukemia.
The risk of developing leukemia increases from the age of 30. Men are affected slightly more often than women and around four percent of those affected are children under the age of 15.

What are the symptoms of leukemia?
In some cases, leukemia comes on suddenly with symptoms and progresses quickly. Doctors then speak of acute leukemia. In other cases, the blood cancer develops slowly and insidiously. Then it is chronic leukemia.
Symptoms of acute leukemia
In acute leukemia, the symptoms develop relatively quickly. Symptoms of both acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) include:
• Reduced performance
• Persistent fever
• Night sweats
• Fatigue
• Weight loss
• Bone and joint pain (especially in children with ALL).
Over time, people’s bodies produce increasing amounts of immature, non-functional white blood cells, which crowd out healthy blood cells. This causes further signs of leukemia accordingly. The lack of red blood cells leads to anemia. For example, those affected suffer from:
• Paleness
• Fast heart rate
• Shortness of breath
• Dizziness.
The lack of blood platelets (thrombocytes) in acute leukemia often causes an increased tendency to bleed. Those affected often have gum or nosebleeds, for example. When injured, it takes longer than usual for a wound to stop bleeding. In addition, these people get more bruises (hematoma) – another typical sign. Severe platelet deficiency (thrombocytopenia) causes red hemorrhages in the skin, so-called petechiae.
Leukemia often weakens the immune system against infections. As a result, the sufferers suffer from stubborn infections such as inflammation in the oral cavity that does not heal well. The reason for this is that the body has too few functional white blood cells, which in turn serve to fight off infections. The immune system in leukemia is therefore weakened overall.
Other possible leukemia symptoms are:
• Painlessly swollen lymph nodes
• Enlarged liver and spleen
• Skin rashes
• Gum overgrowth.
Symptoms of chronic leukemia
Chronic leukemia begins insidiously. In the first few months or even years, many patients have no symptoms. Some only report general symptoms such as fatigue and reduced performance. However, most of those affected do not initially recognize these as signs of leukemia. That’s why they don’t go to the doctor. Only in an advanced stage do symptoms of chronic leukemia develop that resemble an acute course.
In chronic myeloid leukemia (CML), a distinction is made between three phases in which the disease becomes increasingly aggressive. This is also reflected in the leukemia signs:
• Chronic phase : Here the number of white blood cells is abnormally high (leukocytosis) and the spleen is enlarged (splenomegaly). The latter often causes a feeling of pressure in the upper left abdomen. Other leukemia symptoms in this phase include fatigue and reduced performance.
• Acceleration phase (transitional phase) : The number of leukocytes continues to increase. At the same time, the number of red blood cells and platelets decreases. Typical symptoms of CML are pale skin, tachycardia, shortness of breath and frequent nose and gum bleeding. Night sweats and fever sometimes also occur. The liver is progressively enlarged.
• Blast crisis (blast attack) : In this last phase of the disease, the bone marrow releases large quantities of immature precursors of blood cells (so-called myeloblasts and promyelocytes) into the blood. This causes symptoms similar to those of acute leukemia. Most patients die soon.
Chronic lymphocytic leukemia (CLL) also progresses slowly. Although the term “leukemia” is in the name, it is not blood cancer, but a special form of lymph gland cancer (malignant lymphoma).
What types of leukemia are there?
The four main types of leukemia are:
| Leukemia type | Remarks |
| Acute myeloid leukemia (AML) | • Starts quite suddenly and progresses rapidly. • Most common acute leukemia. • About half of the patients are older than 70 years. |
| Chronic myeloid leukemia (CML) | • Slow, insidious course (except in the last stage: blast crisis). • Mean age of onset at 50 to 60 years. • Very rare in children. |
| Acute Lymphocytic Leukemia (ALL) | • Starts quite suddenly and progresses rapidly. • Most common of all forms of leukemia. • Especially in children (ALL is the most common type of cancer in children); adult patients mostly older than 80 years. |
| Chronic Lymphocytic Leukemia (CLL) | • Slow, gradual course. • Most common leukemia in adults; mean age of onset at 70 to 75 years. • Does not belong to the “real” leukemias, but to lymph gland cancer (malignant lymphomas). |
There are also other types of leukemia that are very rare. One example is hairy cell leukemia.
The so-called myelodysplastic syndromes (MDS) are related to leukemias. These are also chronic diseases of the bone marrow, in which too few functional blood cells are produced. Symptoms are similar to chronic myeloid leukemia. But they are less pronounced at first. In about 25 to 30 percent of those affected, the myelodysplastic syndrome sooner or later develops into a fully developed leukemia, namely acute myeloid leukemia.
Myeloid leukemia
Myeloid leukemias originate from the so-called myeloid progenitor cells in the bone marrow. Normally, healthy red blood cells, platelets, and granulocytes and monocytes develop from these progenitor cells. The last two are subsets of white blood cells.
However, when myeloid progenitor cells degenerate and begin to grow out of control, myeloid leukemia develops. Depending on their course, physicians differentiate between acute myeloid leukemia (AML) and chronic myeloid leukemia (CML). Adults in particular suffer from both forms of blood cancer. AML is significantly more common than CML.
Lymphocytic leukemia
Lymphatic leukemias originate from different blood cell precursors than myeloid blood cancer: here the so-called lymphatic precursor cells degenerate. From them the lymphocytes emerge. This subgroup of white blood cells is very important for the targeted (specific) defense against foreign substances and pathogens (specific immune defence).
Here, too, one speaks of acute lymphocytic leukemia (ALL) or chronic lymphocytic leukemia (CLM), depending on the course of the disease. ALL is the most common form of blood cancer in children and adolescents. CLL, on the other hand, typically occurs in older adults. It is only referred to as “leukemia” (blood cancer) because of its course. CLL is actually a form of lymph gland cancer – it is one of the so-called non-Hodgkin lymphomas.
Hairy cell leukemia
Hairy cell leukemia (or hairy cell leukemia) is a very rare cancer. The same applies to them as to chronic lymphocytic leukemia: the “leukemia” part of the name only indicates that the disease progresses like blood cancer. However, it is attributed to lymph gland cancer (more precisely: non-Hodgkin lymphoma).
The name “hair cells” comes from the fact that the cancer cells have hair-like extensions.
Hairy cell leukemia only occurs in adults. Men are affected much more frequently than women. The chronic disease is not very aggressive. Most sufferers have a normal life expectancy.
Leukemia in children
Leukemia is primarily a disease of adults: They make up about 96 percent of all patients. When childhood leukemia develops, it is almost always acute lymphocytic leukemia (ALL). Acute myeloid leukemia (AML) follows in second place. Chronic leukemias are very rare in children.
If acute blood cancer in childhood is discovered and treated early, the chances of recovery are good. In comparison, acute leukemia in adults tends to have a poor prognosis.
How is leukemia treated?
Leukemia treatment is individually tailored. Various factors play a role in this. In addition to the age and the general state of health of the person concerned, it is above all the course of the disease, i.e. whether the leukemia is acute or chronic.
Treatment of acute leukemia
After the diagnosis of “acute leukemia” chemotherapy usually begins as soon as possible. It is considered the most important therapy method for acute blood cancer. The affected person receives special medication, so-called cytostatics (chemotherapeutic agents). They stop cancer cells (and other rapidly dividing cells) from growing. The damaged cells also stop multiplying. The body’s own control mechanisms recognize the diseased cells and break them down in a targeted manner.
The doctor usually administers the cytostatics via an infusion directly into the vein. Occasionally, sufferers take them as pills. Cytostatics are available individually or in combination and in different dosages. In this way, the chemotherapy can be individually adjusted. The treatment also takes place in cycles : the patient receives the cytostatics on one day or on several days in a row. Then there is a break in treatment (days to months) before a new cycle begins. Most sufferers receive an average of four to six such chemotherapy cycles.
Basically, the therapy runs in three phases, which together can extend over months and years:
- Induction therapy: Those affected receive strong chemotherapy that eliminates as many cancer cells as possible and relieves the most severe symptoms. Treatment is usually inpatient in the hospital.
- Consolidation therapy: It is designed to “consolidate” the success of the induction therapy. Appropriately adapted chemotherapy eliminates the remaining cancer cells as far as possible.
- Maintenance therapy: This is about stabilizing the success of the treatment and preventing a relapse. The maintenance therapy is designed very differently from person to person. In this phase, those affected often take cytostatics such as azacitidine in tablet form for at least a year.
Induction therapy is sometimes so successful that practically no cancer cells can be detected in the patient’s blood or bone marrow. Doctors then speak of a remission. But it does not mean that the leukemia is cured. It is possible that individual cancer cells survived. Therefore, further therapy steps (consolidation therapy) are necessary.
After the maintenance therapy, follow-up care follows: the doctor regularly examines the blood and bone marrow. In the event of a relapse, the cancer cells can be detected early in this way. Follow-up care is also about treating any side effects and long-term consequences of previous chemotherapy.
Other therapy options
Sometimes a stem cell transplant is also part of the leukemia treatment. Stem cells are the “mother cells” from which all blood cells in the bone marrow are made. Prior to transplantation, it is necessary to use high-dose chemotherapy (and possibly whole-body radiation) to destroy virtually all of the patient’s bone marrow and (hopefully) all of the cancer cells.
The doctor then transfers healthy stem cells, just like in a transfusion. The cells settle in the medullary cavities of the bones and produce new, healthy blood cells.
For such a stem cell transplant, the transplanted stem cells often come from a healthy donor (allogeneic stem cell transplant). More rarely, stem cells are taken from the patient themselves, which were taken from them before the bone marrow was destroyed (autologous stem cell transplantation). The therapy method is primarily considered when other treatments (especially chemotherapy) are not effective enough or the patient suffers a relapse.
Many people with acute lymphocytic leukemia (ALL) receive radiation therapy in addition to chemotherapy. On the one hand, the doctor irradiates the head as a preventative measure, since the cancer cells more frequently invade the brain. On the other hand, he uses radiation to treat malignant lymph nodes, for example in the chest area.
Treatment of chronic leukemia
Chronic myeloid leukemia (CML) is usually diagnosed by doctors in the chronically stable phase of the disease. The doctor then prescribes so-called TYROSINE KINASE INHIBITORS (such as imatinib). These drugs have a very specific effect on blood cancer cells: they inhibit growth signals in the cells. Ideally, this keeps the disease at bay for many years. The tyrosine kinase inhibitors are available as oral tablets, and most patients take them for life.
At the same time, the doctor regularly checks the blood and bone marrow. If, for example, the blood values or the patient’s condition deteriorates, this indicates that the CML is moving to the next phase (acceleration phase). The doctor then changes the drug treatment: He prescribes other tyrosine kinase inhibitors. In many patients, the disease can be returned to a chronically stable phase.
If that doesn’t work, allogeneic stem cell transplantation may be an option – i.e. the transplantation of healthy, blood-forming stem cells from a donor. So far, this is the only form of therapy that offers a chance of completely curing chronic myeloid leukemia. However, it is very risky. Doctors therefore carefully weigh up the benefits and risks of treatment for each patient beforehand.
At every stage of the disease, it is possible for the patient’s condition to deteriorate significantly within a short period of time. Then doctors speak of a blast crisis. As with acute leukemia, those affected receive mostly intensive chemotherapy. In this way, doctors try to quickly suppress the signs of the disease. If the condition has improved and stabilized again, a stem cell transplant may make sense.
Some patients with CML are treated with interferons. These are messenger substances with which the cells of the immune system communicate with each other. They are able to inhibit the growth of cancer cells. However, like chemotherapy, interferons are usually less effective in CML than the tyrosine kinase inhibitors described above.
But this is not always the case: tyrosine kinase inhibitors work best in patients whose cancer cells have what is known as the “Philadelphia chromosome”. This is what a characteristically altered chromosome 22 is called. It can be detected in more than 90 percent of all CML patients. The remaining patients do not have the altered chromosome. Therefore, treatment with tyrosine kinase inhibitors often does not work so well for them. Then it is sometimes necessary to change the therapy and use interferons, for example.
Many patients with chronic lymphocytic leukemia (CLL) do not require treatment for a long time. Only when the blood values deteriorate or symptoms occur in an advanced stage do doctors initiate therapy – individually adapted to each individual patient.
For example, many patients receive chemotherapy plus so-called monoclonal antibodies (immunochemotherapy or chemoimmunotherapy). The artificially produced antibodies specifically bind to the cancer cells and thereby mark them for the immune system. Doctors occasionally use both forms of therapy individually.
If the cancer cells show certain genetic changes, treatment with tyrosine kinase inhibitors may make sense. These drugs block an abnormal enzyme that promotes the growth of cancer cells.
If other treatments don’t work or there is a later relapse, (allogeneic) stem cell transplantation is sometimes an option. However, this risky treatment is only suitable for young people or people whose general health is good.
Accompanying measures (supportive therapy)
In addition to leukemia treatment using chemotherapy, radiation therapy and others, supportive measures are also very important. They serve, for example, to reduce symptoms of the disease and the consequences of treatment. This improves the well-being and quality of life of the patients enormously.
For example, nausea and vomiting are common and very uncomfortable side effects of chemotherapy for leukemia (and other cancers). They can be relieved with special medication (antiemetics).
Increased susceptibility to infection is also a serious problem in leukemia. Both the disease itself and chemotherapy weaken the immune system, making it less able to fight pathogens. This favors infections, which then sometimes run very seriously, sometimes even being life-threatening. Therefore, careful hygiene and an environment that is as germ-free as possible are very important for people with leukemia. Many are also given antibiotics to prevent or treat bacterial infections. Active ingredients against fungal infections are so-called antimycotics.
Other complaints can also be treated in a targeted manner, for example anemia with blood transfusions and pain with suitable painkillers.
What is the prognosis for leukemia?
For many people with leukemia, the chances of survival are significantly better today than they were several years or decades ago. Modern therapies often improve the chances of recovery. If the cancer is too advanced, treatment will at least relieve many patients’ symptoms, thereby increasing their survival time.
In individual cases, the prognosis for leukemia depends on various factors. First and foremost are the type of cancer and the stage of the disease at the time of diagnosis. How well the patient responds to therapy also has an impact on the prognosis. Other factors that influence life expectancy and chances of recovery in leukemia are the age and general condition of the patient and any concomitant diseases.
Chances of recovery
Is leukemia curable? Many patients and their families ask themselves this question. In principle, acute leukemia can be cured. The earlier the disease is discovered and treated, the greater the chances of recovery. This is especially true for younger patients.
Without treatment, most patients survive the diagnosis of “acute leukemia” for only about three months. With treatment, 95 percent of children and 70 percent of adults with acute lymphocytic leukemia (ALL) are alive five years after diagnosis. For acute myeloid leukemia (AML), the five-year survival rate is 40 to 50 percent in patients under 60 years of age and 20 percent in those over 60 years of age.
Even if the cancer can be pushed back, it often comes back later, even after months and years. In the case of an early relapse in particular, the chances of recovery decrease. Leukemia patients then have to be treated again. Doctors sometimes choose more aggressive therapy or other treatment methods.
In chronic leukemia, the cancer cells multiply more slowly than in acute forms of cancer (exception: blast crisis in CML) – and usually for years. Therefore, the treatment is usually less intensive, but must be continued in the long term. In general, chronic leukemia cannot be cured (this chance only exists with risky stem cell transplantation). In many patients, however, the therapy alleviates the symptoms and slows the progression of the chronic leukemia.
How do you diagnose leukemia?
While chronic leukemia usually remains symptom-free for a long time, acute forms begin relatively suddenly and progress quickly. Symptoms such as reduced performance, paleness, tachycardia, frequent nosebleeds or persistent fever also occur with many other diseases, some of which are harmless. That is why they are not always taken seriously. With such complaints, however, there is always a suspicion of leukemia. Therefore, those affected should definitely see a doctor.
The first point of contact if blood cancer is suspected is the general practitioner. If necessary, he or she will refer the patient to a specialist, for example a specialist in blood and cancer diseases (haematologist or oncologist).
Consultation with the doctor and physical examination
The doctor first collects the medical history (anamnesis). To do this, he asks how the person in question feels in general, what complaints they have and how long they have existed. Information about any other illnesses that currently exist or have occurred in the past are also important. The doctor will also inquire, for example, about the medication the person is taking and whether there is a family history of cancer.
This is followed by a thorough physical examination. Among other things, the doctor listens to the lungs and heart, measures the blood pressure and feels the liver, spleen and lymph nodes. The results help the doctor to better assess the general condition of the patient.
Blood test
A blood test is important if you suspect leukemia or a related disease. The doctor does a small blood count and a differential blood count (complete blood count). The small blood count indicates, among other things, the number of white blood cells (total number), red blood cells and platelets. The so-called hematocrit (Hkt value) can be determined, which provides information about the proportion of all solid components in the blood, for example the red blood cells.
Furthermore, the doctor determines the so-called MCH value, which indicates how much hemoglobin.
For the differential blood count, the different subgroups of the white blood cells are measured individually. The doctor also examines the blood cells under the microscope and thus assesses their appearance, which is altered in leukemia. Pathologically altered blood values such as an increased number of white blood cells and a lack of red blood cells are possible indications of leukemia. However, they are also typical of many other diseases. Therefore, further differential diagnostic tests are usually required.
In addition to the blood cells, the doctor also assesses other blood parameters in the laboratory, such as kidney values and liver values. These values indicate how well these two organs are working. If leukemia is confirmed in the further course and the patient’s kidney and/or liver values are poor, this must be taken into account when planning therapy.
The laboratory also checks whether the blood shows signs of infection with bacteria, viruses or fungi. These germs may also be responsible for some symptoms, such as an increased number of white blood cells, fever and fatigue.
Bone marrow puncture
With any suspicion of leukemia, it is necessary to closely examine the patient’s bone marrow. For this purpose, the doctor takes a bone marrow sample, usually from the pelvic bone (bone marrow puncture), with a special needle under local anesthesia. In the laboratory, the doctor examines the number and appearance of the bone marrow cells. With typical changes, leukemia can be clearly identified. Sometimes even the type of the disease can be determined. The doctor also examines the cells for changes in their genetic material. For example, there is the “Philadelphia chromosome” in chronic myeloid leukemia.
Adults and older children are usually given a local anesthetic before the bone marrow is removed. A short anesthetic is advisable for smaller children. The whole puncture usually only takes about 15 minutes and can be performed on an outpatient basis.
Further investigations
Once the diagnosis of leukemia is confirmed, further investigations are often necessary. They show whether other body regions and organs are also affected by the cancer cells. The general condition of the patient can also be better assessed with such examinations. This is important for therapy planning.
For example, the doctor examines internal organs (spleen, liver, etc.) using ultrasound. He may also do a computed tomography (CT) scan. This imaging method is also suitable for assessing the bones. This is important if the doctor suspects that the cancer cells have spread not only to the bone marrow but also to the bone itself. Other examination methods are nuclear spin or magnetic resonance imaging (MRT) or scintigraphy.
In acute lymphocytic leukemia (ALL) and some subtypes of acute myeloid leukemia (AML), the cancer cells sometimes invade the brain or meninges. Possible signs of this are headaches and neuronal failures such as blurred vision and paralysis. Then the doctor takes a sample of the spinal fluid (lumbar puncture) and analyzes it in the laboratory. MRI is also helpful to detect brain cancer.
What causes of leukemia?
The causes of the various types of blood cancer have not yet been clearly clarified. However, experts have identified several risk factors that promote the development of leukemia. These include:
Genetic predisposition: The risk of leukemia is slightly increased if cancer has occurred more frequently in one’s own family. In addition, certain genetic diseases make you more susceptible to blood cancer. For example, people with trisomy 21 (” Down syndrome “) have a 20-fold higher risk of acute myeloid leukemia (AML) than people without this genetic mutation.
Age: The development of acute myeloid leukemia (AML) is influenced by age: the risk of developing the disease increases with age. The same applies to chronic myeloid leukemia (CML) and chronic lymphocytic leukemia (CLL). In contrast, acute lymphocytic leukemia (ALL) occurs mainly in childhood.
Smoking: Experts estimate that smoking is responsible for about ten percent of all leukemia cases. For example, active smokers have a 40 percent higher risk of developing acute myeloid leukemia (AML) than people who have never smoked. In ex-smokers, the risk of developing the disease is still increased by 25 percent.
Lonizing rays: Such ionizing rays are also used in radiation therapy for cancer. However, they not only kill the cancer cells, as desired, but sometimes also damage the genetic material in the healthy cells. In rare cases, patients develop a radiation-related second cancer as a result.
X-rays are also ionizing. However, experts assume that an occasional X-ray examination does not trigger leukemia. However, X-rays should only be taken when absolutely necessary. Because the damage that the radiation causes in the body usually accumulates over the course of life.
Chemical substances: Various chemical substances increase the risk of leukemia. These include, for example, benzene and other organic solvents. Insecticides (insecticides) and plant protection products (herbicides) are also suspected of promoting blood cancer.
This connection is certain for certain drugs that are actually used to treat cancer (such as cytostatics): they promote the development of leukemia in the long term. Doctors therefore carefully weigh up the benefits and risks of such drugs before using them.
Viruses: Certain viruses (HTL viruses I and II) are involved in the development of a very rare form of leukemia. This so-called human T-cell leukemia mainly affects people in Japan. This blood cancer variant is very rare in Europe.
According to the current state of knowledge, all other types of leukemia (AML, CML, ALL, CLL et cetera) develop without any involvement of viruses or other pathogens.
How to prevent leukemia?
Since the actual causes of leukemia are largely unclear, it is difficult or impossible to determine any preventive measures. Doctors advise minimizing the risk factors. A healthy lifestyle and avoiding tobacco and excessive alcohol, for example, can help here. Get regular check-ups, especially if you are older. For example, early, non-specific signs can be clarified in good time.
