Atrial fibrillation (AF), is a heart rhythm disorder characterized by frequent and irregular heartbeats.
This is the most common arrhythmia in the world. It is estimated that atrial fibrillation affects up to 3% of the world’s adult population. With age, the prevalence of atrial fibrillation increases and among people over 60 years of age can reach 60%.
The disease causes a decrease in quality of life due to repetitive heartbeat attacks and is associated with increased mortality.
The disunity of the work of the atria and ventricles during atrial fibrillation leads to a decrease in cardiac output by 20-30% due to the absence of an atrial contribution to cardiac output and inadequate filling of the left ventricle with blood.
Thus, long-term atrial fibrillation leads to an expansion of the heart cavities, a pronounced decrease in the pumping function of the heart, the occurrence of insufficiency of the mitral and tricuspid valves, which leads to an increase in heart failure.
One of the most serious complications of atrial fibrillation is stroke. This is due to the fact that with atrial fibrillation in the heart, extremely favorable conditions arise for the formation of blood clots: the atria cease to contract normally, which, in turn, leads to stagnation of blood and thrombus formation in the heart.
Blood clots leave the heart with the flow of blood and can block blood flow in the arteries of the brain or other organs.
Atrial fibrillation increases the risk of stroke by 5 times, and among patients with dysfunction of the heart valves – 20 times, in comparison with patients without arrhythmias.
Causes of atrial fibrillation
Diseases of the cardiovascular system:
- Pathology of the mitral valve of the heart (congenital and acquired defects)
- Arterial hypertension (systolic blood pressure more than 140 mm Hg)
- Rapid heart rate (for example, in athletes after exercise)
- Ischemic heart disease, heart attack (atherosclerotic lesions of the coronary arteries)
- Pericarditis (inflammation of the bursa – pericardium)
- Myocarditis (inflammatory lesion of the heart muscle – myocardium).
Other causes:
- Thyrotoxicosis (hyperfunction of the thyroid gland)
- Diabetes mellitus (high blood glucose)
- Infectious diseases
- Genetic predisposition
- Nervous shock or stressful situation
- Intense strenuous physical activity
- Alcohol, nicotine and drug abuse
- Intoxication with various drugs.
Atrial fibrillation symptoms
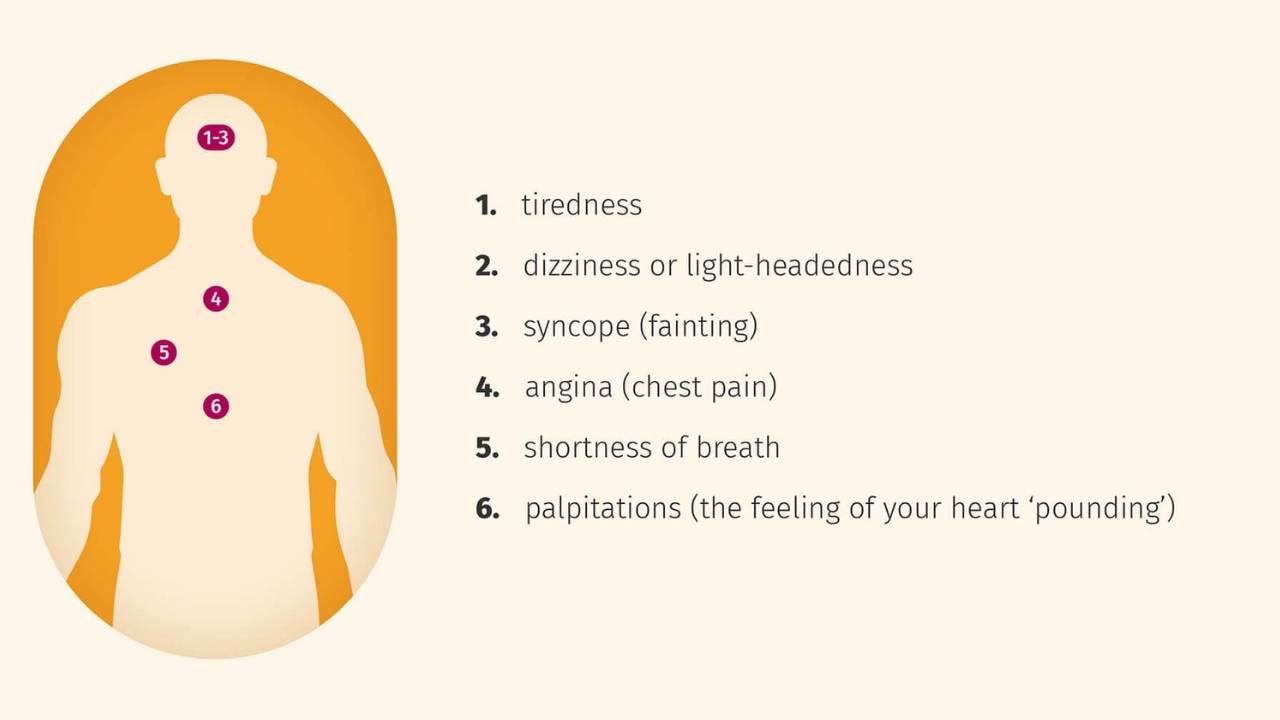
The most common symptoms of atrial fibrillation are:
- interruptions in the heart
- sinking heart
- frequent irregular heartbeat
- chest pain
- dizziness
- fainting or short-term loss of consciousness
- shortness of breath, lack of air
- dyspnea
- increased fatigue
- general weakness.
Often, atrial fibrillation is asymptomatic and is detected by chance on an ECG or during Holter monitoring.
Atrial fibrillation classification (ESCGuidlines):
- Paroxysmal form – a sudden onset of AF, lasting from several minutes to 7 days, recovers on its own (more often within 24-48 hours).
- Persistent form – atrial fibrillation lasting from 7 days to 1 month. It does not recover on its own, but there are indications and the possibility of cardioversion.
- Long-term persistent form – atrial fibrillation lasting more than 1 month, persisting or recurrent, despite attempts at cardioversion.
- The permanent form is atrial fibrillation, in which cardioversion is contraindicated, has not been performed, or has been unsuccessful.
The prevalence of atrial fibrillation is 6% in elderly and senile people and about 2% in the entire population. In 6-10% of patients with coronary artery disease, the disease is complicated by atrial fibrillation, and in patients with mitral heart disease requiring surgical treatment, atrial fibrillation develops in 60-80% of cases. Observations indicate a significant increase in the incidence of this arrhythmia.
In patients with atrial fibrillation, mortality is approximately 2 times higher than in patients with sinus rhythm.
Dissociation of the work of the atria and ventricles leads to a decrease in cardiac output by 20-30% due to the absence of an atrial contribution to cardiac output, as well as inadequate filling of the left ventricle with blood.
Thus, long-term atrial fibrillation leads to the development of dilated cardiomyopathy, which is accompanied by expansion of the cardiac cavities, pronounced systolic dysfunction of the left ventricle (decreased ejection fraction), the occurrence of mitral and tricuspid regurgitation (reverse flow of blood), which leads to an increase in heart failure.
The presence of atrial fibrillation leads to stagnation of blood and thrombus formation in the left atrial appendage with a high risk of blockage of the cerebral arteries, the great arteries of the upper and lower extremities (systemic circulation), and blood vessels supplying internal organs.
Every sixth stroke occurs in a patient with atrial fibrillation. The risk of such a complication in patients with atrial fibrillation is 5 to 7 times higher than in people without arrhythmia.
In patients with heart defects of rheumatic etiology complicated by atrial fibrillation, the risk of developing acute cerebrovascular accident (ACVA) is 17 times higher than in patients without atrial fibrillation.
Diagnosis
The main method for diagnosing atrial fibrillation is electrocardiography (ECG) and Holter monitoring – continuous long-term (for 1 – 7 days) ECG recording.
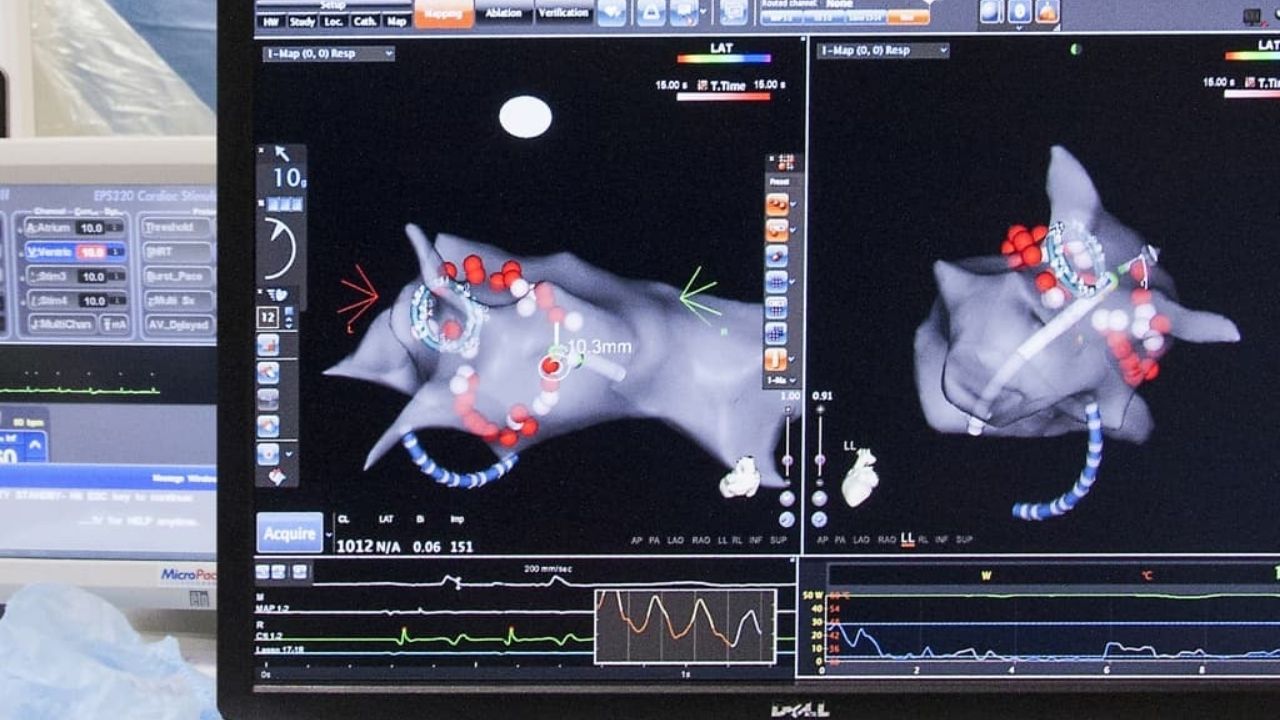
If the diagnosis of AF is confirmed and the indications for endovascular catheter ablation of AF are determined, the patient undergoes an electrophysiological study (EPI) with the identification of zones of ectopic foci and the construction of a map of these zones.
Treatment
Conservative treatment of atrial fibrillation
Atrial fibrillation is a risk factor for ischemic stroke resulting from the formation of blood clots in the left atrial cavity.
The primary agents in the treatment of atrial fibrillation are drugs that prevent blood clots. They are prescribed by a doctor, tk. monitoring of the blood coagulation system is required.
These funds are indicated for almost all patients who suffer from atrial fibrillation, regardless of whether arrhythmia is constantly present or seizures occur (paroxysmal arrhythmia).
The risk of stroke is the same for both chronic arrhythmias and paroxysmal arrhythmias.
In patients with a paroxysmal form of atrial fibrillation, the issue of preventing the onset of arrhythmia attacks is being resolved. If an attack occurs for the first time, antiarrhythmic drugs are not prescribed.
Drugs may be recommended to control heart rate and improve the tolerance of recurrent paroxysms of arrhythmias.
Antiarrhythmic drugs are also not prescribed if the patient’s arrhythmia attacks are asymptomatic and do not reduce his quality of life.
In case of recurrence of rhythm disturbances and deterioration of the tolerance of paroxysms, the cardiologist-arrhythmologist, together with the patient, decides on the appointment of antiarrhythmic drugs or surgical treatment of arrhythmia (catheter ablation).
With the development of a protracted attack of atrial fibrillation, which did not go away on its own, it is necessary to consult a specialist cardiologist-arrhythmologist, who will choose the most appropriate method for arrhythmia relief for the patient.
The technique of medicamentous restoration of normal heart rhythm, as well as the procedure for restoring the rhythm by the method of electrical cardioversion, has been worked out.
To restore the rhythm, a certain drug preparation is required, the scheme of which will be determined by the doctor, based on the individual characteristics of the course of the disease.
With the advent of the latest highly effective antiarrhythmic drugs, preference is given to medication rhythm restoration.
With the transformation of the paroxysmal form of atrial fibrillation into a chronic form, the main task is to control the heart rate.
In the presence of tachysystole (high heart rate), drugs are prescribed that reduce the heart rate, the primary of which are beta-blockers.
An integral part of the therapy of atrial fibrillation is the treatment of the disease that provoked the rhythm disturbance – ischemic heart disease, heart failure, arterial hypertension, thyroid disorders and others.
It is necessary to consult a cardiologist-arrhythmologist in case of:
- development of an attack of atrial fibrillation for the first time in life
- the development of the next attack of arrhythmia, which cannot be stopped by the usual means
- ineffectiveness of previously prescribed antiarrhythmic therapy.
Radiofrequency catheter ablation
In the event of symptomatic paroxysms of atrial fibrillation, according to modern recommendations, surgical treatment (catheter ablation) can be offered to patients even before antiarrhythmic drugs are prescribed as an alternative to drug treatment.
The efficiency of catheter ablation of atrial fibrillation in most centers around the world is 60-80%. The effectiveness of the intervention is significantly increased by eliminating factors contributing to the development of arrhythmias, such as high blood pressure, overweight, alcohol consumption, etc.
During the procedure, special catheters are inserted into the heart through large vessels (subclavian and femoral veins), through which a radio-frequency current is supplied, affecting the source of arrhythmia.
The operation is electrophysiologically grounded and anatomically oriented. Based on the theory of multiple circles of macro re-entry (circulation of impulse), formed around anatomical structures: the mouths of the pulmonary veins and coronary sinus, superior and inferior vena cava, appendages of the left and right atria, openings of atrioventricular valves.
The operation involves the isolation of these formations and the interruption of the pathways.
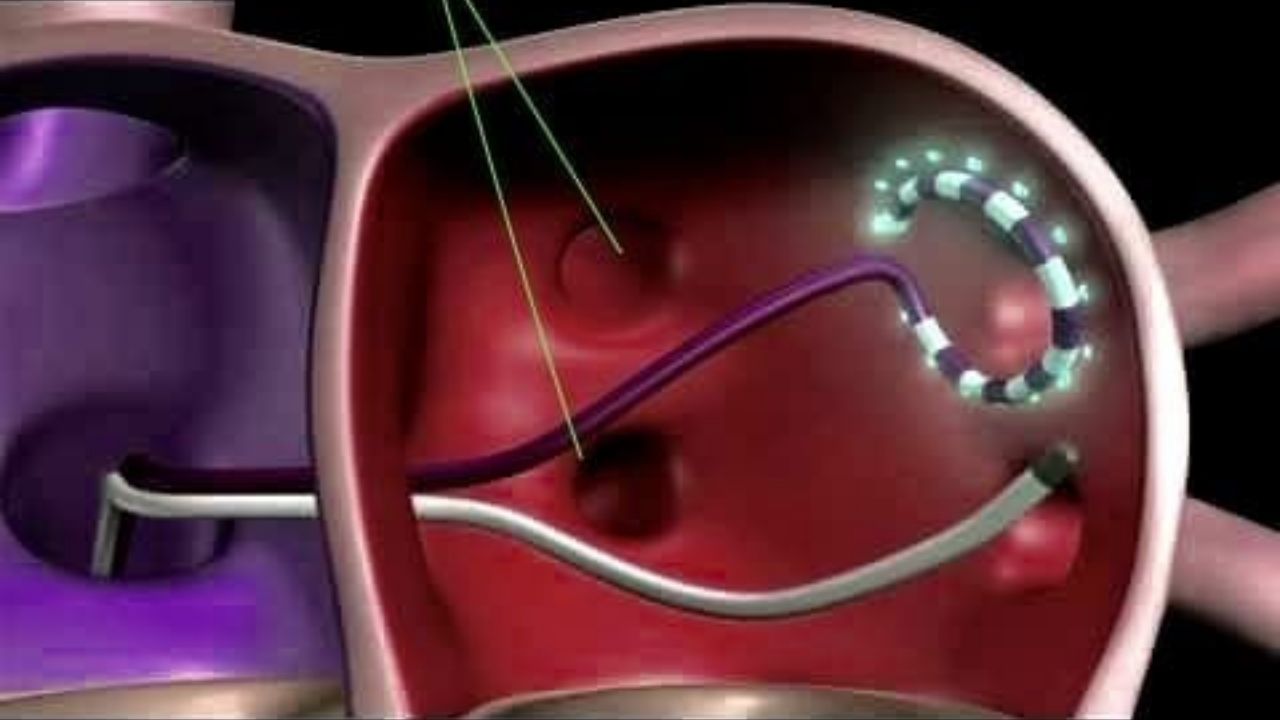
The procedure is performed under X-ray control. The intervention is performed under intravenous (general) anesthesia.
The duration of the procedure is 2-3 hours, depending on the clinical situation.
The main goal of the intervention is to eliminate atrial fibrillation. However, it is not possible to achieve a complete cure in all cases, especially within long-term arrhythmia or its chronic forms.
The use of a hybrid approach – surgical treatment in combination with the intake of antiarrhythmic drugs – can significantly improve the quality of life of patients by reducing the number of attacks and the severity of arrhythmia symptoms.
In the postoperative period, for 3 months, patients are shown the use of drugs that prevent the formation of blood clots, for the prevention of ischemic strokes and antiarrhythmic drugs.
The need for further drug treatment is determined by the attending arrhythmologist.
However, catheter ablation of atrial fibrillation may not always be performed. The procedure is contraindicated in the presence of blood clots in the cavities of the heart, as this contributes to the occurrence of ischemic stroke.
To determine the indications and contraindications for surgical treatment, it is necessary to consult an arrhythmologist.